IS THERE A NEED FOR ESTABLISHING A FORMAL NEPHROLOGIST-DIRECTED PRIMARY CARE PROGRAM IN DIALYSIS UNITS?
Khaja H. Mujtaba Quadri, MD and Sameer Omar Huraib, MD
Division of Nephrology & Hypertension, Department of Medicine
King Fahad National Guard Hospital (KFNGH),
E-mail: mujtabaquadri@hotmail.com,
Riyadh, Saudi Arabia
| DISCUSSION BOARD |
INTRODUCTION
Nephrologists have traditionally provided "primary care" to their dialysis patients. One survey of practising nephrologists revealed that 90 percent of "responders" provided primary care to their dialysis patients.
ADVANTAGES OF A FORMAL PROGRAM
Patients dialyzed on a standard thrice weekly schedule often seek advice on primary care issues from their treating physician/delegate or nurse. Thus, it appears, prudent that a number of primary care interventions can be scheduled in the dialysis unit on dialysis days. Additionally, by having an annual time-table format, specific interventions can be spread over the entire year to accommodate the large dialysis population in certain units.
Moreover, once nurses are familiarized to the structure of such a program, the probability of missing important interventions diminishes, for instance annual history and physical examination. The thrice a week schedule also helps in implementing certain interventions logistically viz immunization specifically influenza, pneumovax and DT boosters may be given on alternate days in the "immunization week" before the onset of the "flu season". Finally, since most of the "interventions" are pre-requisites of a renal transplant program, patients may automatically get worked up for transplantation, barring specific additional requirements.
DISADVANTAGES
Patients may potentially perceive these primary care interventions as an additional "burden" and may not comply with visits "outside" the unit. This may be particularly true if procedures are felt to be cumbersome and long "on dialysis days" and requiring additional transportation/visits on "non-dialysis days".
The King Fahad National Guard Hospital Program for Primary Care of Hemodialysis Patients
This program was conceived in the summer of 2000 and initiated in September 2000 as a pilot program to be reevaluated in subsequent years. A preliminary report follows subsequently.
AIMS
In the absence of formal primary care guidelines for patients with end stage renal disease, our program aims to introduce a comprehensive annual time-frame for providing routine and dialysis specific primary care services, "modified" from the US Preventive Services task force recommendations.
METHODS
After informed consent all 102 chronic hemodialysis patients at King Fahad National Guard Hospital, Riyadh were enrolled in the primary care program in September 2000.7 The outline of the "annual time-table" format was approved by Hospital Administration and Chairpersons/ Divisional Heads of all involved departments/ divisions. A comprehensive "inservice" was conducted for the physicians and nurses responsible for routine care of the hemodialysis patients. Fourteen age/sex specific appropriately indicated primary care tests, exams, immunizations and interventions were performed according to our modified annual time-table. Figure (A).
Figure A : PRIMARY HEALTH CARE (PHC) PROGRAM FOR KING FAHAD NATIONAL GUARD HOSPITAL DIALYSIS PATIENTS
| Age | Sept. | Oct. | Nov. | Dec. | Jan. | Feb. | March | April | May | June | July | Aug. |
| 18-34 | ||||||||||||
| 35-49 | Fasting lipid profile (annually) |
|||||||||||
| 50-64 | Fasting lipid profile (annually) +PSA (annually) |
Stool occult blood (annually) |
For 60+ (2 yearly) EYE (vision/ glaucoma) ENT (2 yearly) |
EYE ENT |
Flex sigmoi- doscopy q 3 yearly morning |
Flex sig. afternoon |
Flex sig. evening | |||||
| 65-79 | Fasting lipid profile (annually) +PSA (annually) |
Stool occult blood (annually) |
EYE ENT (Sat, Mon, Wed) shift |
EYE ENT (Sun, Tue, Thurs) shift) | Flex sig. morning (shifts) |
Flex sig. afternoon (shifts) |
Flex sig. evening (shifts) | |||||
| 18-34 | PAP Smear (if married) (yearly x2 then q 3 yrs) |
PAP Smear (if married) (yearly x2 then q 3 yrs) |
||||||||||
| 35-49 | Fasting lipid profile (annually) |
For 40+ Breast exam (annually) |
Breast exam | PAP Smear | PAP Smear | |||||||
| 50-64 | Fasting lipid profile (annually) |
Stool occult blood (annually) |
For 60+ (2 yearly) EYE (vision/ glaucoma) ENT (2 yearly) |
EYE ENT |
Breast exam | Breast exam | Mammogram yearly x2 (then q 2 yearly) |
PAP Smear (Sat, Mon, Wed) shift |
PAP Smear (Sun, Tue, Thurs) shift |
Flex sig. morning |
Flex sig. afternoon |
Flex sig. evening |
| 65-79 | Fasting lipid profile (annually) |
Stool occult blood (annually) |
EYE ENT (Sat, Mon, Wed) shift |
EYE ENT (Sun, Tue, Thurs) shift) |
Breast exam (Sat, Mon, Wed) shift |
Breast exam (Sun, Tue, Thurs) shift |
Mammogram yearly x2 (then q 2 yearly) |
Flex sig. morning shifts |
Flex sig. afternoon shifts |
Flex sig. evening shifts | ||
| P3, P4, CA++ (ionized), AL, HbAlc, Mg, Fe, TIBC, Ferritin, PTH, pre/post BUN, CBC, HBV profile, HCV Fasting lipid profile (all diabetics) |
P3, P4, CA++ (ionized) HbAlc, pre/post BUN, CBC, Vaccination 1. Influenza (annual) 2. Pneumovax (lifetime once) 3. DT (q 10yrs) 4. Hep B status follow-up |
P3, P4, CA++ (ionized) HbAlc pre/post BUN, CBC, PRA Arterial Venous BUN Peripheral *EYE clinic for all diabetics (Sat, Mon, Wed) |
P3, P4 CA++ (ionized), AL, HbAlc, Mg, Fe, TIBC, Ferritin, PTH, pre/post BUN, CBC, EYE clinic for all diabetics (Sun, Tue, Thurs) |
P3, P4, CA++ (ionized) HbAlc pre/post BUN, CBC, History/ Physical Sat/Mon/ Wed shift |
P3, P4, CA++ (ionized) HbAlc pre/post BUN, CBC, PRA Arterial Venous BUN Peripheral History/ Physical Sun/Tue/ Thurs shift |
P3, P4 CA++ (ionized), AL, HbAlc, Mg, Fe, TIBC, Ferritin, PTH, pre/post BUN, CBC, HBV profile, HCV |
P3, P4, CA++ (ionized) HbAlc pre/post BUN, CBC, U/S kidneys (annual) Hand x-rays (q2 yr) (Sat, Mon, Wed) shift |
P3, P4, CA++ (ionized) HbAlc pre/post BUN, CBC, PRA Arterial Venous BUN Peripheral U/S kidneys (annual) Hand x-rays (q2 yr) (Sun, Tue, Thurs) shift |
P3, P4 CA++ (ionized), AL, HbAlc, Mg, Fe, TIBC, Ferritin, PTH, pre/post BUN, CBC, HBV profile, HCV Dental (yearly) (morning shift) |
P3, P4, CA++ (ionized) HbAlc pre/post BUN, CBC, Dental (yearly) (afternoon shift) |
P3, P4, CA++ (ionized) HbAlc pre/post BUN, CBC, PRA Arterial Venous BUN PeripheralDental (evening shift) |
Dialysis specific monitoring and multi-disciplinary meetings were continued as per our pre-existing standards. Appropriate therapeutic interventions and case-specific referrals were performed. Each area of intervention was deemed to be highly successful (more than 66% or two-thirds compliance), moderately successful (50% to 66% compliance) or unsuccessful (less than 50% compliance).
RESULTS: Tables I and II and Figure B
Month | Primary intervention | Sex | Age | N |
Positive (Abnormal) | Negative (Normal) |
| Sept | 1. Lipid profile | M F | 35-79 35-79 |
41 43 | 8(19.51%) 12(27.40%) | 33(80.49%) 31(72.60%) |
| 2. PSA | M | 50-79 |
27 | 2(7.40%) | 25(92.60%) | |
Oct | 3. Vaccination (influenza DT, pnemovax) | M/F | 12-88 | 102 |
90(89%) completed | 12(11%) incomplete |
| 4. Stool occult blood | M F | 50-79 50-79 |
32 34 | 1(3.1%) 1 (2.9%) | 23(71.8%) *8 missed (25.1%) 28(82.35%) *5 missed (14.5%) |
|
Nov | 5. Eye Exam |
M/F | 60-79 | 37 |
14(37.85%) (DM retinopathy 6, | 0 *23 missed appointment (62.15%) |
| Dec | 6. ENT exam | M/F | 60-79 | 37 | 5(13.51%) High freq deafness – 3 Others - 2 | 7(18.91%) *25 missed appointment (67.6%) |
| Jan/ Feb | 7. Annual history/physical | M/F | 12-88 | 102 | 68 (66.6%) completed | 34(33.3%) incomplete |
| 8. Breast exam | F | 40-79 | 41 | 4(9.7%) | 25(60.97%) *12 refused (29.3%) | |
| March | 9. Mammography | F | 50-79 |
34 | 3 Increased density 2, nodule 1 (8.82%) | 20(58.8%) *11 refused (32.4%) |
|
Month |
Primary intervention |
Sex |
Age |
N |
Positive |
Negative |
|
April/ May |
10. Pap smear (yrly x 2 then q 3 yrs) |
F |
18-64 |
24 |
0 (0%) |
13 (54.1%) No show 11 (45.9%) |
|
11. Ultrasound kidneys (annual) |
M/F |
12-88 |
102 |
Not applicable |
Not applicable *unable to schedule in pilot year |
|
|
12. Hand x-rays (two yearly) |
M/F |
12-88 |
102 |
39(38.2%) Osteodystrophy 12 Osteopenia 23 Osteoporosis 3 Others 1 |
19 (18.6%) No show 44(43.2%) |
|
|
Jun – Aug. |
13. Flexible sigmoidoscopy |
M |
50-79 |
31 |
2 (6.4%) (Rectal & sigmoid polyp) |
8 (25.8%) No show/refused 21 (67.8%) |
|
F |
50-79 |
34 |
1 (2.9%) (rectal polyp) |
2 (5.8%) No show/refused 31 (91.3%) |
||
|
14. Dental exam |
M/F |
12-88 |
102 |
Not applicable |
Not applicable *unable to schedule in pilot year |
|
|
N.B. Some discrepancy in numbers in various age groups in different months reflect the changes as a result of additional new patients, travel, morbidity/mortalityTable I |
||||||
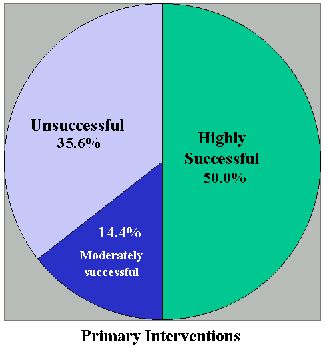
CONCLUSIONS
We were successfully able to implement 9/14 (65%) of our targeted primary care interventions in our hemodialysis population in our pilot year. Amongst our unsuccessful interventions 5/14 (35%), only failure of our flexible sigmoidoscopy program may have long-term consequences, when extrapolated to the general population. This may involve renewed efforts at patient education in subsequent years. Our annual "time-table" appears to provide a practical, efficient and administratively acceptable format for providing nephrologist directed primary care to the hemodialysis population, hitherto not described in the literature. Future data from this primary care program may yield the long term effects on morbidity and mortality in our dialysis population.
DISCUSSION
We at KFNGH believe that for the hemodialysis population already burdened with a thrice a week dialysis schedule, nephrologist directed primary care is a multidisciplinary process and needs to be spread over the entire year. Success in implementing this process is largely dependent on working around the dialysis schedule. Hence, most of our interventions were accomplished in the dialysis unit, e.g. history and physical exam, breast exams, PSA screen, immunization program, lipid profiling and stool occult blood. Where our success was modest or uninspiring was in areas where patients had to undergo specific appointments and scheduling in addition to their thrice weekly dialysis, e.g. pap smear and flexible sigmoidoscopy. Some of the areas, perhaps eye and ENT screening needed to be scheduled on dialysis days, in the absence of which very poor compliance was noted. The long term impact and costs could be looked at over subsequent years, but in general most interventions implemented are well established cost-effective screening tools.
SUMMARY
We have introduced an annual time-table format for addressing the "primary care" needs of the hemodialysis population. For 102 patients enrolled, fourteen interventions adapted for the dialysis population from the US Preventive Services Task Force recommendations were implemented successfully in 65% areas in our pilot year, which include important features like annual history & physical exam, breast exam, mammography, pap smear, lipid profile, adult specific immunization and stool "occult" blood. Flexible sigmoidoscopy program was unsuccessful in our pilot year.
ACKNOWLEDGEMENT TO CO-INVESTIGATORS
Junaid Qureshi, Hammad Raza, Fahad Al Kanhal, Carol Lum, Bella May Loria, Catherine Powell, Danlami Z. Tanimu, Ghormullah Al Ghamdi, Ahmed Al Flaiw, Zuhair M. Abunijem and all involved departments and secretarial assistance, particularly Ma. Sofia Claridad.
REFERENCES
1. Bender FH, Holley JL. Most nephrologists are primary care providers for chronic dialysis patients: results of a national survey. AJKD 28(1):67-71, July 1996)
2. Gipson D, Katz LA, Stehman-Breen C. Principles of dialysis: special issues in women. Seminars in Nephrology 19(2):140-7, March 1999
3. Neu AM, Fivush BA. Immunization for pediatric dialysis patients. Adv. Renal Replacement Therapy, 7(3):239-46, July 2000
4. Sarnak MJ, Levey AS. Cardiovascular disease and chronic renal disease: a new paradigm. AJKD. 35(4 Suppl 1):S117-31, April 2000
5. Holley JL. Nephrologists as primary care providers: a review of the issues. AJKD, 31(4):574-83, April 1998
6. US Public Health Service 1994
7. Quadri KHM, Kanhal F, Qureshi JI, Raza H, Lum C, Loria BM, Powell B, Tanimu DZ, Ghamdi G, Al Flaiw A, Abunijem ZM and Huraib SO. A primary care program for hemodialysis patients. Abstract JASN, A1229 September 2001. Poster presentation at joint ASN/WCN Annual meeting 2001.