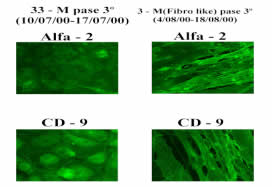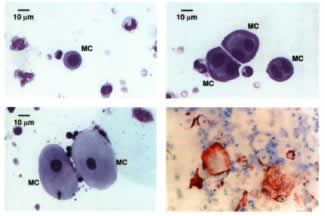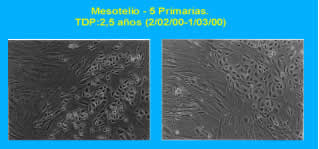
The main objective of this talk is to provide some insights on the early diagnosis of a process that develops in some long-, medium-term PD patients, and which final consequences may be very severe for the membrane and for the patient. The transcendence of early diagnosis is then clear. Early diagnosis of Risk Factors for ESP development, is probably the best way to prevent it Diagnosis Key Factors -Clinical background -Peritoneal functional abnormalities or changes -Peritoneal effluent composition changes -Peritoneal cytology changes -Peritoneal anatomy changes Image techniques Peritoneal biopsy Clinical Background and signs suggestive that something is happening in the peritoneum Glucose abuse, UF deficit and/or severe peritonitis Intolerance to usually tolerated infusion volume Further decrease of deficient UF capacity Intestinal occlusive (or sub-) signs and symptoms Unexpected hemoperitonuem Peritoneal functional abnormalities Ultrafiltration failure type I shifting towards type II Progressive Decrease of Urea-MTC/Creatinine-MTC Ratio Lack of response (UF recovery) to a four-week resting period Markedly Low UF with icodextrin Peritoneal effluent composition CA 125 (Mesothelial cell mass) Hyaluronic Acid (Healing) Phospholipids(Mesothelial cell integrity) Factor VIII(Endothelial cell mass) Collagen Peptides(Collagen turnover) TGF-b (Pro-fibrotic activity) VEGF(Angiogenesis) Peritoneal cytology Peritoneal anatomy: Image techniques and biopsy -Patched Absence of Mesothelial cells -Mild Chronic Inflammatory Infiltrates -Neoangiogenesis -Proliferation of Fibroblasts -Increase of ECM -Vascular wall thickening and hyalinosis -Fibrosis Image Techniques: …..Too late Conclusions The Combination of Peritoneal Functional Sequential Studies With Cytology Observations and Mesothelial Fine Changes, directly or in culture Represents the Best Alternative for ESP Early Diagnosis
DISCUSSION BOARD
16/11/01
Haga clic aquí para ver las imagenes