
CLASS, ACTIVITY AND CHRONICITY INDICES, AND alpha-SM ACTIN EXPRESSION AS PROGNOSTIC FACTORS IN LUPUS NEPHRITIS.
Cuan Ravinal R. 1, Costa R.S. 1, Pastorello M.T.1, Coimbra T.M.2, 4Department of General Pathology, Faculty of Medicine of Triângulo Mineiro,
Coelho E.B.3 Dantas M. 3, dos Reis M.A.4

1 Department of Pathology, 2 Department of Physiology,
3 Division of Nephrology, Faculty of Medicine of Ribeirão Preto,
University of São Paulo, Ribeirão Preto - SP. Brazil.
Uberaba - MG. Brazil.
E-mail: cuan@rpa.fmrp.usp.br
| DISCUSSION BOARD |
INTRODUCTION
Lupus nephritis results from an acute inflammatory and immunological response to renal immune complex deposition 1. The acute response is characterized by activation of circulating leukocytes and renal parenchymal cells, triggering the production of pro-inflammatory cytokines and growth factors 1, 2. This response is followed by a chronic phase, which is characterized by excessive deposition of collagen and other extracellular matrix macromolecules, and by progression to renal fibrosis 1-4.
Studies of the predictive value of renal biopsy in lupus nephritis have evaluated the prognostic significance of the World Health Organization (WHO) criteria and of the presence of active or chronic lesions, or both 5. A composite of scores for those items that reflect disease activity, and therefore potentially reversible lesions, is the activity index that includes inflammatory and proliferative changes. Similarly, a composite of scores for those items that reflect chronic irreversible lesions including sclerosis and atrophic and fibrotic changes is called chronicity index 6. The activity and chronicity indices provide semiquantitative information regarding the severity of acute or chronic injury to the glomerular, tubulointerstitial, and vascular compartments of the kidney 4, 7.
Clinicopathological studies have clearly shown that fibrosis involving the glomerular, vascular, and especially, the intertistial compartments of the kidney is the strongest marker for end-stage renal disease. In most of cases, progression to end-stage renal failure occurs over a period of a few to many years 8.
Renal fibrosis (along with glomerulosclerosis) is the final common pathway of a relatively uniform response of the kidney to sustained inflammation independent of its origin 9. The ultimate anatomical feature of glomerular sclerosis is the accumulation of extracellular matrix in the glomerulus and collapse of capillary lumina 9, 10. Tubulo-interstitial scarring is characterized by tubular atrophy and an accumulation of interstitial matrix, which may emanate from fibroblasts or tubular cells themselves and occurs with any number of different primary diseases, whether immune, metabolic or degenerative 7, 9, 10.
Recent studies have demonstrated that progressive glomerulonephritis is associated with phenotypic changes in glomerular cells. alpha-Smooth Muscle actin (alpha-SM actin) is expressed normally by vascular smooth muscle cells and by stromal fibroblastic and mesangial cells in pathological conditions leading to fibrosis including renal scarring 11-14.
In various types of glomerular injury, the mesangial cells acquire the characteristics of myofibroblasts, which may in fact be injurious to the glomerulus. Like myofibroblasts in other tissues, the mesangial cell acquires smooth muscle cell-like properties, characterized by de novo expression of a-smooth muscle actin, and the development of fibroblast-like properties characterized by the production of interstitial collagens in addition to normal mesangial matrix constituents 12, 13.
The aims of the present study were to correlate histological features (class, activity and chronicity indices) with the progression of lupus nephritis, and to determine the pathological role of myofibroblasts in lupus nephritis outcome.
SUBJECTS AND METHODS
Patients and clinical evaluation
We studied renal biopsies from 86 patients with lupus nephritis. All patients had at least four manifestations of lupus as described by the American College of Rheumathology 1. Kidney biopsies were obtained from the files of the Department of Pathology, Medical School of Ribeirão Preto, and were used in accordance with the principles of the Declaration of Helsinki. The involved procedures were also approved by the local University Ethics Committee (The Brazilian National Council of Health, law 196/96).
Clinical and laboratory data were obtained from the medical records of the patients using a protocol as previously reported 15. The parameters assessed in the approach to lupus nephritis were serum creatinine, serum albumin, total serum protein, 24 h proteinuria., examination of urinary sediments, serum complement profile, serum protein electrophoresis, and renal biopsy.
The following classification of the outcome forms of lupus nephritis were considered during the clinical follow-up of the outcome 15: (i) clinical remission: proteinuria below 200 mg/day with normal renal function; (ii) clinical improvement: regression of nephrotic or nephritic syndrome or acute renal failure or reduced proteinuria with stable renal function; (iii) unchanged: unchanged clinical and/or laboratory data during the course of the disease, (iv) clinical worsening: aggravation of nephrotic or nephritic syndrome, acute renal insufficiency or increased proteinuria with normal renal function; (v) chronic renal insufficiency: creatinine of 1.5 mg/dL or more. We considered remission or clinical improvement to indicate a favorable clinical outcome and clinical worsening and chronic renal insufficiency to indicated an unfavorable clinical outcome.
Patients with lupus nephritis were considered to have been treated when they received corticosteroids (methylprednisone or prednisone) combined or not with immunosuppressive drugs as cyclophosphamide, regardless of the schedule used.
Morphological Evaluation
Morphological evaluation was performed by renal biopsy using common light microscopy and immunofluorescence microscopy 15. Tissue obtained by renal biopsy from 86 patients with lupus nephritis and control sections from preserved renal areas of kidney from nephrectomized patients were fixed in Bouin's solution, embedded in paraffin, cut into 4-mm-thick sections, and stained with hematoxylin and eosin (HE), Masson trichrome and methenamine silver, and the specimens were prepared for immunofluorescence microscopy 15. Renal lesions were classified according to the histologic criteria outlined in the revised WHO classification system and the scores for individual active lesions (activity index) and chronic, irreversible lesions (chronicity index) were calculated 6, 16, 17.
Immunohistochemical Studies
The immunohistochemical studies were performed using a murine monoclonal antibody to an NH2-terminal synthetic form of alpha-SM actin (DAKO Corporation, Glostrup, Denmark). Four-mm sections of biopsy tissue embedded in paraffin were processed by the indirect immunoperoxidase technique as previously described 18. Serial 4-mm-thick sections were incubated overnight at 4º C with 1:1000 alpha-SM actin monoclonal antibody. The avidin-biotin-peroxidase complex procedure (Vectastain, Vector Laboratories, Burlingame, CA, USA) was employed as the detection system. Chromogen development was performed with 3,3'-diaminobenzidine (DAB) (Sigma Chemical Co., St Louis , Mo, USA), and the material was counterstained with Harris hematoxylin or methyl green, dehydrated, and mounted.
Negative controls consisted of the omission of primary antibody in the reaction. Glomerular expression of alpha-SM actin was graded semi-quantitatively according to Alpers et al 14, modified: 0, no staining; 1, trace mesangial staining, 2, weak segmental mesangial staining, usually involving a small minority of the glomeruli present; 3, strong segmental mesangial staining, usually involving a majority of the glomeruli present; and 4, strong diffuse mesangial staining, usually involving all glomeruli present. The alpha-SM actin immunoreaction in the tubulo-interstitium of the renal cortex was scored as follows: 0, absent staining; +, weak staining with focal distribution; ++, moderate staining with focal distribution; +++, strong staining with focal distribution or weak and diffuse; and ++++, strong and diffuse.1
When data distribution was normal, the values were expressed as mean ± standard error. Proportions were determined using the standard chi-square test (c2 ) with Yates correction or Fisher's exact test. Significance difference was accepted if p<0.05.
Eighty-six patients were studied, 77 women (89.6%) and 9 men (10.4%). Mean age of onset of lupus nephritis was 25.8 ± 10.2 years. Sixty-six patients were white (76.7%) and 20 (23.3%) were black . We did not observe a significant correlation between clinical outcome of lupus nephritis and sex, age and race (p > 0.05). Eighty-two patients had renal disease at the time of SLE diagnosis. Median follow-up time was 75.5 ± 57.3 months. Histological examination showed the following classes of lupus nephritis: 2 patients (3.5%), class IIa; 8 patients (9.3%), class IIb; 16 patients (18.6%), class III; 25 patients (29.1%), class IV; 15 patients (17.4%), class V, and 19 patients (22.1%) had mixed pattern nephritis. The clinical outcome of lupus nephritis was distributed as follows: 25 (29.0%) patients with clinical improvement (CI), 35 (40.6%) patients with unchanged clinical outcome (UCC), 14 (16.4%) patients with clinical worsening (CW), and 12 (14.0%) patients with chronic renal insufficiency (CRI).
Clinical course of patients with lupus nephritis as a function of WHO class, activity and chronicity indices in class III and IV, and alpha-SM actin scores in glomeruli and tubulo-interstitial area, are showed in Tables 1 to 7, and Figure 1. Only the parameters WHO class IV patients (p = 0.011), and chronicity index for WHO class III patients (p = 0.027) showed statistical significance when compared to the clinical outcome of lupus nephritis. In our study, WHO class IV compared to the other classes, and high chronicity index for WHO class III patients compared to low chronicity index were found to be poor microscopic prognostic factors in lupus nephritis.
RESULTS
Table 1 Clinical outcome of patients with lupus nephritis as a function of WHO classes (n = 86 patients).
Clinical outcome/ Classes II a II b III IV* V MP
Total Remission 0 0 0 0 0 0 0
Improvement 1 3 2 3 6 9 25 Unchanged 2 4 10 8 8 7 35
Worsening 0 1 4 3 1 2 14
CRI 0 0 0 11 0 1 12
Total 3 8 16 25 15 19 86
WHO, World Health Organization; MP, mixed pattern nephritis;
CRI, chronic renal insufficiency; *p = 0.011.Table 2 Clinical outcome of patients with WHO class III lupus nephritis as a function of activity
and chronicity indices (n = 16 patients).
Clinical outcome/Activity index/Chronicity index* 0-8 9-16 17-24 0-3 4-12 Remission 0 0 0 0 0 Improvement 2 0
0 2 0 Unchanged 8 2 0 9 1 Worsening 3 1 0 1 3 CRI 0 0 0
0 0 Total 13 3 0 12 4
WHO, World Health Organization; CRI, chronic
renal insufficiency.
Clinical outcome versus activity index p = 0.750,
Clinical outcome versus chronicity index *p = 0,027. Table 3 Clinical outcome of patients with WHO class IV lupus nephritis as a function of activity and
chronicity indices (n = 25 patients).
Clinical outcome/Activity index/Chronicity index* 0-8 9-16 17-24 0-3 4-12 Remission 0 0 0 0 0 Improvement 0 1
2 3 0 Unchanged 3 2 3 7 1 Worsening 3
0 0 2 1
CRI 2 7 2 9 2 Total 8
10 7 21 4
WHO, World Health Organization; CRI, chronic renal insufficiency.
Clinical outcome
versus activity index p = 0.316,
Clinical outcome versus chronicity index p = 0.621.
Table 4 alpha-SM actin expression in glomeruli of patients with WHO class III lupus nephritis
as a function of clinical outcome (n = 16 patients).
Clinical outcome/Score 0 1 2 3 4 Total Remission 0 0 0 0 0 0 Improvement 1 0 1 0 0 2 Unchanged 4 1 3 2 0 10 Worsening 3 1 0 0 0 4 CRI 0 0 0 0 0 0 Total 8 2 4 2 0 16
WHO,World Health Organization; CRI, chronic renal insufficiency;
p = 0.504, considering favorable outcome (remission plus improvement), unchanged,
and unfavorable outcome (worsening plus CRI).
Table 5 alpha-SM actin expression in the tubulo-interstitial area of patients
with WHO class III lupus nephritis as a function of clinical outcome
Clinical outcome/Score 0 + ++ +++ ++++ Total Remission 0 0 0 0 0 0 Improvement 2 0 0 0 0 2 Unchanged 7 2 0 1 0 10 Worsening 3 1 0 0 0 4 CRI 0 0 0 0 0 0 Total 12 3 0 1 0 16
WHO, World Health Organization; CRI, chronic renal insufficiency;
p = 1.000, considering favorable outcome (remission plus improvement),
unchanged, and unfavorable outcome (worsening plus CRI).
Table 6 alpha-SM actin expression in glomeruli of patients
with WHO class IV lupus nephritis as a function of clinical outcome (n = 25 patients).
Clinical outcome/Score 0 1 2 3 4 Total Remission 0 0 0 0 0 0 Improvement 1 1 1 0 0 3 Unchanged 4 0 1 2 1 8 Worsening 0 0 2 1 0 3 CRI 5 2 0 3 1 11 Total 10 3 4 6 2 25
WHO, World Health Organization; CRI, chronic renal insufficiency;
p = 0.447, considering favorable outcome (remission plus improvement),
unchanged, and unfavorable outcome (worsening plus CRI). Table 7 alpha-SM actin expression in the tubulo--interstitial area of patients
with WHO class IV lupus nephritis as a function of clinical outcome
(n = 25 patients).
WHO, World Health Organization; CRI, chronic renal insufficiency;
Clinical outcome/Score
0 + ++ +++ ++++ Total Remission 0 0 0 0 0 0 Improvement 2 0 1 0 0 4 Unchanged 3 1 0 1 3 7 Worsening 0 2 0 0 1 3
CRI 0 3 3 2 3 11
Total 5 6 4 3 7 25
p = 0.304, considering favorable outcome (remission plus improvement),
unchanged, and unfavorable outcome (worsening plus CRI).
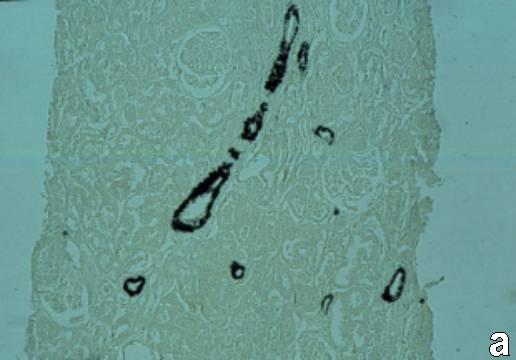
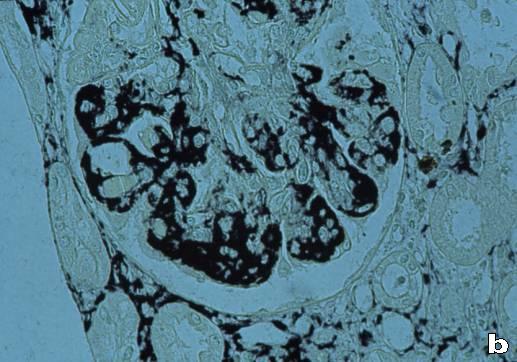 Figure 1- alpha-SM actin score in the renal cortex of patients with lupus nephritis. (a) A human control. Normal detectable levels of alpha-SM actin expression in arteriole walls. (b) WHO class IV lupus nephritis. Mesangial alpha-SM actin score 4, and tubular-interstitial area score ++++.
Figure 1- alpha-SM actin score in the renal cortex of patients with lupus nephritis. (a) A human control. Normal detectable levels of alpha-SM actin expression in arteriole walls. (b) WHO class IV lupus nephritis. Mesangial alpha-SM actin score 4, and tubular-interstitial area score ++++.
DISCUSSION
Genetic factors are important in lupus nephritis, with a strong racial preponderance. The prevalence and mortality of lupus are ten times higher in black women than in whites 5. In contrast to the literature, our study showed a higher incidence of lupus nephritis among white patients (76.7%).
Many clinical parameters have been used to estimate the prognosis of lupus nephritis. Young age at onset of systemic lupus nephritis, male gender, and black race are associated with increased renal failure and a poor prognosis of renal disease 5. In our study, sex, age and race were not significantly associated with unfavorable clinical course (UCC).
Concerning the frequency of WHO classes in lupus nephritis, several studies (cited in 6) showed approximately 25% of renal biopsies specimens with WHO class III, 37% with WHO class IV, and 13% with WHO class V. Our study showed 18.6% from class III, 29.1% from class IV, and 17.4% from class V. Furthermore, we found 3.5% of the patients from class IIa, 9.3% from class II b, and 22.1% from mixed pattern nephritis.
Some investigators have described as features predictive of remission the WHO class IV lupus nephritis 19, 20. By other hand, other investigators reported that patients with WHO classes III and IV lupus nephritis have a poor outlook in terms of morbidity, clinical presentation, and worse prognosis 21-27. McLaughlin et al, in a study of 123 patients with lupus nephritis, found that survival rates were higher in those with minimal glomerular lesions, intermediate in those with focal and diffuse proliferative lesions, and lower in those with diffuse glomerulosclerosis 28. In our study, 56% of patients from class IV lupus nephritis had an UCC showing a worse prognosis for class IV compared to the other classes. In the same way, our results showed a worse prognosis for high chronicity index at least in the class III patients, in agreement with the study of McLaughlin.
Austin et al 29, 30 found that certain histologic features of renal biopsy when semiquantitated and expressed into either activity index and chronicity index may provide useful prognostic information on renal survival in patients with lupus nephritis. The activity index was found to be a relatively weak predictor of renal failure outcome. The chronicity index has been found to yields mixed unequal results, with some investigators finding them prognostically useful while others find that they do not predict outcome 31. Schwartz et al 32, in a study of 83 patients, showed that both indices are insufficient as therapeutic guides and add little to the management of the patient with severe lupus nephritis. Our results revealed that only the chronicity index is significantly correlated with clinical outcome of class III lupus nephritis patients.
In our opinion, the activity index does not have correlation with the clinical outcome because it is the expression of lesions that are potentially reversibles, and also the patients may present different outcomes to the same therapeutic approach. On the other hand, we have been unable to explain the lack of correlation between the clinical outcome and the chronicity index to WHO class IV lupus nephritis. Since the WHO class IV usually has a worse prognosis compared to the other classes, we speculate that this worse prognosis might dissemble the prognostic value of the chronicity index in our class IV patients.
The expression of alpha-SM actin in glomeruli has been assumed to reflect the activation and proliferation of mesangial cells and the consequent increase in collagen content. Besides, interstitial myofibroblasts represent a key step in renal fibrogenesis, have been associated with a poor prognosis in experimental and clinical glomerulonephritis and are the strongest predictors of progressive renal insufficiency 9-11, 20. Alpers et al 14 showed that glomerular expression of alpha-SM actin was correlated with the expression of proliferating cell nuclear antigen (PCNA) in several types of human glomerulonephritis. These investigators, also showed that most of the patients with proliferative diffuse lupus nephritis presented the higher scores of alpha-SM actin. Similar results were show by Hurtado et al.33. In our study, we did not find a significant correlation between the clinical outcome of WHO classes III and IV lupus nephritis and the score of alpha-SM actin expression in glomeruli and in tubulo-interstitial area. Our data shows that neither the glomerular or the tubulo-interstitial score for alpha-SM actin expression can predict individual outcomes of kidney function in lupus nephritis.
In summary, sex, age, race, and alpha-SM actin expression in the glomeruli or in tubulo-interstitial area in WHO classes III and IV were no correlated with clinical follow-up outcome in lupus nephritis. By the other hand, an UCC was correlated with WHO class IV compared to the other classes. In the same way, high chronicity index may predict a worse outcome for renal failure, but only for WHO class III patients.
REFERENCES