
RENAL INVOLVEMENT IN MIXED CRYOGLOBULINEMIA
Franco Ferrario
E-mail: Franco.Ferrario@oscb.sined.net
Renal Immunopathology Center
San Carlo Borromeo Hospital
Milan. Italia
| DISCUSSION BOARD |
Introduction
The pattern of glomerular involvement differs from that of idiopathic type I membranoproliferative glomerulonephritis and from that of the diffuse proliferative glomerulonephritis of systemic lupus eritematodes because of some characteristics:
b) the frequent presence, especially during episodes of acute nephritic syndrome of the so-called “intraluminal thrombi”, which are amorphous, eosinophilic, PAS positive deposits of variable size and diffusion, lying against the inner side of the glomerular capillary wall and often completely filling the capillary lumen
Sometimes these huge intraluminal deposits and the subendothelial deposits are revealed by electron microscopy as having a specific microtubular structure that is identical to that of the in-vitro cryoprecipitate of the same patients. This structure consists of cylinders that are 100 to 1000 µm long and have an hollow axis, appearing in cross section like anular bodies (5-7)
The identity of the deposits with the circulating IgG-IgMk cryoglobulins has been confirmed by demonstration in renal biopsy specimens of the same idiotype of the circulating monoclonal rheumatoid factor (8).
c) the double contoured appearance of the glomerular basement membrane which, at electron microscopy examination, appears to be due to the interposition of monocyte/macrophages between the basement membrane and the endothelial cells or the newly formed basement membrane-like material. Double contours are more diffuse and evident than in idiopathic membranoproliferative glomerulonephritis in which they are due to the prevalent interposition of mesangial cells. This difference in the composition of double contour might explain why it can disappear in cryoglobulinemic glomerulonephritis at a later stage of less clinical activity. Moreover, this milder mesangial involvement might explain why glomerular segmental and global sclerosis is less severe than in other types of idiopathic or secondary membranoproliferative glomerulonephritis (1). Electron microscopy also shows monocyte/macrophages in close contact with the subendothelial and intraluminal deposits, involved in their degradation.
Mesangial sclerosis is found in late stages in the central area of the glomerular lobules (lobular glomerulonephritis) in a minority of patients. In other cases mesangial sclerosis is a late and usually mild feature.
In some cases, the typical pattern of cryoglobulinemic glomerulonephritis is lacking, the monocyte infiltration is less consistent, intraluminal thrombi are absent, and a picture of mild segmental mesangial proliferation is found in 20% of patients.
This pattern can be found at presentation of renal disease or later when a re-biopsy is performed after intensive immunosuppressive therapy.
Finally, about 30% of patients with cryoglobulinemic glomerulonephritis have acute vasculitis of small- and medium-size arteries, characterized by fibrinoid nerosis of the arteriolar wall and infiltration of monocytes in and around the wall (8). This renal vasculitis is often associated with other signs of systemic vasculitis, such as purpura or mesenteric vasculitis and can appear in the absence of clear glomerular involvement.
Even when the fibrinoid necrosis of renal arterial walls is severe, focal necrosis of the capillary loops is never present and crescentic extracapillary proliferation is a rare observation (8).
When subendothelial deposits prevail, the immunofluorescence pattern is similar to that found in idiopathic membranoproliferative glomerulonephritis: intense granular, diffuse subendothelial staining of IgM, IgG and C3. The pattern at immunofluorescence microscopy, when massive intraluminal deposits can be seen by light microscopy, is characterized by intense staining of such deposits prevalently by IgM and IgG, commonly associated with faint irregular segmental subendothelial staining of some peripheral loops. In mild segmental mesangial proliferation, only faint, irregular, segmental, parietal staining of some peripheral loops is found by immunofluorescence.
ITALIAN MULTICENTER STUDY ON HCV-CORRELATED CRYOGLOBULINEMIC GLOMERULONEPHRITIS.
The multicenter retrospective study, organized by the Italian Renal Immunopathology Group, made it possible to review the histological pattern of the largest series of Cryoglobulinemic Glomerulonephritis (GN) published to date, and correlate histological features with virological, biochemical and clinical data.
One hundred and forty-five cases with biopsy specimens available for evaluation, including immunofluorescence analysis were recruited.
Representative material for semi-quantitative evaluation of histological changes was obtained in 128 out of 145 cases.
Morphological features
Three patterns could be clearly identified:
1) Mesangial proliferative GN (10 cases, group A) characterized by mild mesangial proliferation and mesangial matrix expansion without endocapillary proliferation and exudation. The glomerular basement membranes were normal.
2) Focal membranoproliferative GN (10 cases, group B) characterized by typical cryoglobulinemic lesions (mesangial proliferation, marked endocapillary proliferation and exudation, double contour appearance of glomerular basement membrane) involving only less than 50% of glomeruli, with the remnant glomeruli quite normal.
In one case some endolumined thrombi were evident. Surprising mesangio-perietal deposits of IgM, IgG and C3 were present, by immunofluorescence, in all glomeruli.
3) Diffuse membranoproliferative GN (108 cases, group C): The majority of patients presented the above mentioned typical features of cryoglobulinemic GN.
In 52% of the cases variable degrees of endolumined thrombi were present, massive in about 20%.
In 30% of the cases a more marked mesangial matrix expansion and sclerosis was evident with a lobular pattern similar to idiopathic membranoproliferative GN.
A marked global glomerulosclerosis (> 50%) was evident only in 15% of cases.
Extracapillary proliferation was very rare (16%) and only characterized by small segmental crescents, without signs of intracapillary necrosis.
By immunofluorescence the deposits were diffuse in the subendothelial side of the capillary walls, prevailing in the endoluminal thrombi in the patients with this morphological feature present at light microscopy.
The presence of variable degrees of interstitial infiltration of inflammatory cells was detected in 60% of cases in both group B and C while in group A was very rare and scattered.
The intensity of infiltrates correlated with the severity of glomerular infiltration.
Focal area of interstitial fibrosis, with tubular atrophy, was present in the majority of cases.
Morphological evidence of vasculitis of small and medium size arteries was evident in 40% of group B and C cases but also in 10% of group A patients.
A mild to severe arterial and arteriolosclerosis was present in about 30% of cases, in all groups frequently not related to patient age.
Clinico-pathological correlations
TAB I reported the main clinical features at Renal Biopsy in the three different morphological patterns.
CLINICAL FEATURES AT RENAL BIOPSY
Morphological Groups A (10) B (10) C (108) AGE 51,5 ± 13,3 55,4 ± 9,7 57,9 ± 10,53 M/F 1,5/1 1/1,5 1/1,3 Interval onset nephropathy-RB (median – months) 5 7 7 S.Creatinine (mgr%) 1,3 ± 0,7 2,5 ± 2,2 2,6 ± 1,8 S.Creatinine >1,5mg% (%pts) 40 30 33 Proteinuria (gr/24h) 2,5 ± 3,0 2,9 ± 2,9 4,0 ± 9,7
Hypertension (%pts) 60 40 66 Hypo C3 (%pts) 20 30 52
Hypo C4 (%pts) 60 60 93
The mean age at biopsy was similar in the three groups, the male sex prevailing in group A with respect to group B and C.
The median interval between the onset of nephropathy and Renal Biopsy was not different in the three groups, suggesting that different severity of morphological lesions is not time related, but probably the consequence of different intensity of pathogenetic mechanisms.
The mean Serum Creatinine was higher in focal and diffuse membranoproliferative GN.
However, 40% of patients with only mesangial GN presented mild renal failure (S. Creatinine > 1,5 mg%), underlying that independently on glomerular inflammation, tubulo-interstitial and vascular lesions could play an important role in renal function of these patients.
The patients of group C showed, respect the other two groups, higher degree of proteinuria, with more than 50% of cases presenting Nephrotic Syndrome, and Hypocomplementemia (especially for C4), expression of more severe activity of renal disease.
Hypertension, sometimes severe, was present in about half of patients in the three groups.
Extrarenal signs of the disease (artralgya, abdominal pain and purpura) were extremely more frequent in group C (80% of pts), again underlying a more active disease in this group of cases with more severe renal damage.
Serum anti-HCV antibodies and HCV-RNA were detected in the majority of patients (90%) without differences among the three groups.
The HCV genotypes more frequently associated to our cryoglobulinemic GNs were 1 b (53%) and 2 (44%) with similar distribution in the three groups.
Follow-up
A mean follow-up of 56±35 months (median 40 months) was available in 117 patients.
In Tab II the clinical features of the three groups at last observation are reported.
CLINICAL FEATURES AT LAST OBSERVATION
Morphological Group A (10) B (9) C (98) Urinary abnormalities (%pts) 60 55 56 Proteinuria (gr/24h) 0,67 ± 0,72 0,74 ± 1,02 0,64 ± 0,75 Nephrotic Syndrome(%pts) - - 13 Chronic renal failure
(% pts) 40 45 31
S.Creatinine (mg%) 2,5 ± 0,8
2,3 ± 1,0 2,3 ± 1,0
Mean follow-up
(months) 44 ± 56 62 ± 56 55 ± 53 Median F.U. 24 30 38
Group A: after a mean follow-up of 44±56 (median 24) 60% of patients presented only mild urinary abnormalities, while 40% showed chronic renal failure (S. Creatinine 2,5 ± 0,8 mg%). 1 patient died from extrarenal symptoms.
Not one patient reached end stage renal failure.
Group B: a mean follow-up of 62±56 months (median 30) was available in 9 patients.
55% of cases presented urinary abnormalities and 45% renal insufficiency (S. Creatinine 2,3 ± 1,6 mg%). Two patients showed a worsening of renal failure while two others an improvement of renal function.
Not one patient died or reached end stage renal failure.
Group C: a mean follow-up of 55 ± 53 months (median 38) was available in 98 cases.
56% of patients presented urinary abnormalities while only 13% still showed Nephrotic Syndrome. Thirteen patients showed a progression of renal failure but twentytwo cases presented an improvement of renal function
At last observation 31% of cases presented chronic renal failure but not one reached end stage renal failure.
13 patients died from extrarenal symptoms.
Discussion
The data of this multicenter study, in a very large cohort of patients, confirmed that the cryoglobulinemic GN is characterized in the great majority of patients by a peculiar type of membrano-proliferative exudative glomerulonephritis (1 – 4), strictly connected with the precipitation of circulating IgG-IgMK cryoglobulins.
The identity of the deposits with the circulating IgG-IgMK cryoglobulins has been confirmed by our demonstration in renal biopsy specimens of the same idiotype of the circulating monoclonal Reumathoid Factors (9).
The main morphological lesions can be variable in intensity from one patient to another but usually they are diffuse with massive monocyte accumulation and frequently huge endoluminal thrombi.
Glomerular segmental and global sclerosis is rather mild and inconstant and end stage renal failure due to sclerosing nephritis is uncommon.
Renal vasculitis, although more frequently present in patients with more acute exudative GN, can also be found in the absence of obvious glomerular damage.
Even when the fibrinoid necrosis of arterial walls was present we never saw lesions of necrotizing-crescentic GN (capillaritis) that is a typical morphological aspect of ANCA-associated renal vasculitis.
The data confirmed that the majority of patients presented urinary abnormality, while Nephrotic Syndrome was present in about 30% of cases and Nephrotic Syndrome in 10% (8 - 10).
A more severe clinical Syndrome (renal failure, higher proteinuria) was prevalent in diffuse and severe forms (group C) but it is important to stress that these symptoms were also present in cases with mesengial patterns, underlying the possible importance of tubulo-interstitial and vascular lesions in determining renal damage.
Our data confirmed the strict association between cryoglobulinemic GN and HCV infection, in particular with genotypes 1b and 2, and the quite constant presence of hypocomplementemia in particular for C4 .
Finally we confirmed, that also taking into account a limited period of observation with respect to others series (8), the renal outcome of cryoglobulinemic GN is good.
Several patients showed improvement of proteinuria and renal function while few cases presented a worsening of renal function without developement of end stage renal failure.
Being a retrospective multicenter study and considering the extreme variability of therapeutic regimes no evaluation of the effect of therapy in the outcome of patients was made.
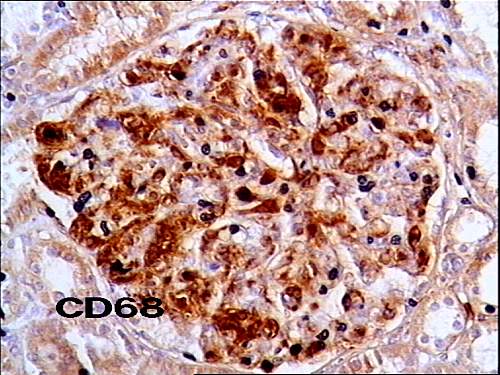
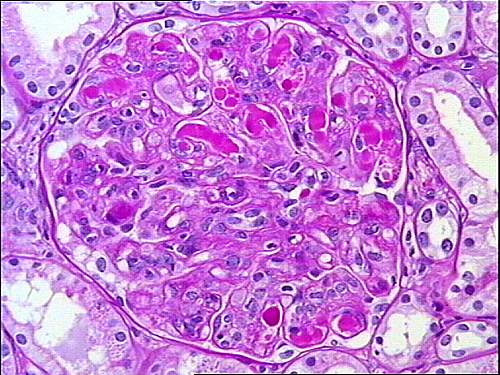 Fig 2: membranoproliferative glomerulonephritis with huge intracapillary
Fig 2: membranoproliferative glomerulonephritis with huge intracapillary
deposits (thrombi) totally filling the capillary lumina (PAS x 250)
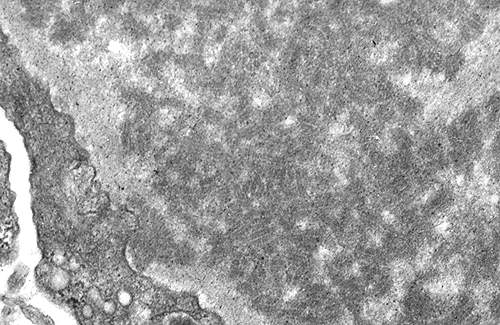 Fig 3: subendothelial deposits showing a specific anular and
Fig 3: subendothelial deposits showing a specific anular and
cylindrical
structure (original magnification x 3600)
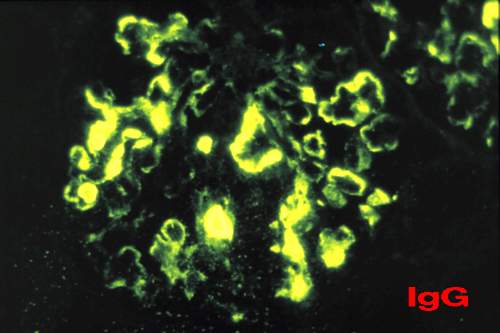 Fig 4: intense staining of deposits filling the capillary lumina.
Fig 4: intense staining of deposits filling the capillary lumina.
Segmental
and irregular parietal deposits (IgG x 250).
1. D’Amico G., Colasanti G., Ferrario F., and Sinico R.A. Renal involvement in essential mixed cryoblobulinemia. Kidney Int 1989, Vol.35:1004-1014.
2. Monga A., Mazzucco G., Barbiano di Belgioioso G., and Busnach G. The presence and possible role of monocyte infiltration in human chronic proliferative glomerulonephritis. Am J Pathol 1979, Vol. 94: 271-284.
3. Ferrario F., Castiglione A., Colasanti G., Barbiano di Belgioioso G., Bertoli S., and
D’Amico G. The detection of monocyte in human glomerulonephritis. Kidney Int 1985,
Vol. 28: 513-519
4. Castiglione A., Bucci A., Fellin G., D’Amico G., and Atkins R.C. The relationship of
infiltrating renal leucocytes to disease activity in lupus and cryoglobulinemic
glomerulonephritis. Nephron 1988, Vol. 50: 14-23
5. Mihatsch M.J., and Banfi G. Ultrastructural features in glomerulonephritis in essential
mixed cryoglobulinemia. In: C. Ponticelli, L.Minetti and G. D’Amico (eds) Antiglobulins,
Cryoglobulins and Glomerulonephritis, Dordrecht, M. Nijhoff, 1986, p.211.
6. Cordonnier D., Martin H., Groslambert P., Micouin C., Chenais F., and Stoebner P.
Mixed IgG-IgM cryoglobulinemia with glomerulonephritis. Immunochemical fluorescent
and ultrastructural study of kidney and in vitro cryoprecipitate. Am J Med 1975, Vol.
59: 867-872.
7. Feiner H., and Gallo G. Ultrastructure in glomerulonephritis associated with
cryoglobulinemia. Am J Pathol 1977, Vol. 88: 145-162.
8. Tarantino A. Campise M., Banfi G., Confalonieri R., Bucci A., Montoli A., Colasanti G.,
Damilano I., D’Amico G., Minetti L., and Ponticelli C. Long-term predictors of survival in
essential mixed cryoglobulinemic glomerulonephritis. Kidney Int 1995, Vol. 47: 618-623
9. Sinico A.R., Winearls CG., Sabadini E., Fornasieri A., Castiglione A., D’Amico G.
Identification of glomerular immune deposits in cryoglobulinema glomerulonephritis.
Kidney Int 1988, 34:1-8
10. Barbiano di Belgiojoso G., Montoli A., Tarantino A., et al. Clinical and histological
correlation in essential mixed cryoglobulinemia (EMC) glomerulonephritis. In: Ponticelli
C., Minetti L., D’Amico G., eds Antiglobulins, cryoglobulins and glomerulonephritis.
Dodrecth: Martinus Nijhoff 1986, 203-10
Correspondence to:
REFERENCES
Franco Ferrario, MD
Renal Immunopathology Center
San Carlo Borromeo Hospital
Via Pio II, 3 20153 Milan – Italy
Tel: +39 2 40222876
Fax: +39 2 40222222
E-mail: Franco.Ferrario@oscb.sined.net