
ACUTE ABDOMEN IN PATIENTS WITH PERITONEAL DIALYSIS.
UTILITY OF LAPAROSCOPY
Moreno Sanz C, PhD., EBSQ.
drmoreno@laparoscopia-online.com
Seoane González JB, PhD. jseoaneg@laparoscopia-online.com
Servicio de Cirugía General. Hospital General "La Mancha-Centro".
Alcázar de San Juan. Ciudad Real. SPAIN.
| DISCUSSION BOARD |
Continuous or chronic ambulatory peritoneal dialysis (CAPD) has become an accepted treatment for end-stage chronic renal failure. It is well known that peritonitis is the most common complication of CAPD. The majority of these cases of peritonitis are catheter related and will usually resolve with antibiotic therapy. Although a single organism usually causes catheter related peritonitis, 6-9% of cases are polymicrobial in origin.
A patient with CAPD can suffer an acute abdomen from gastrointestinal origin and it is a diagnostic challenge for surgeons to identify those patients with multiple enteric organisms isolated from the peritoneal fluid who will benefit from surgical exploration.
Surgical exploration can be performed by means of laparotomy or laparoscopy.
Laparoscopy is fast becoming the preferred surgical approach to a number of different pathologies because it allows them to be diagnosed and treated at the same time. There are also clear advantages for the patient associated with this type of minimally invasive surgery. In emergency abdominal situations, both of the critical components of operative treatment - exploration to identify the causative pathology and performance of an appropiate operation – can often be accomplished via laparoscopy.
The purpose of this conference is to provide an overview about the use of laparoscopy in the diagnosis and treatment of the acute abdomen in patients with CAPD.
DIAGNOSIS OF PERITONITIS IN CAPD PATIENTS
Pain is usually the predominant and presenting feature of peritonitis. Pain in catheter related peritonitis is usually gradual, diffuse, and steady. Nausea, vomiting, fever and an increased white blood cell count are also common. It is well known that in order to elucidate the cause of an acute abdomen, the location, mode of onset and progression, and character of pain must be determined. Nevertheless, the "spread and lavage" effect of the dialysis fluid in these patients can vary the development of typical symptoms in the most common causes of acute abdomen. Patients with symptoms of diffuse abdominal pain that fail to localize the quadrant of maximum pain are common and suspicion of appendicitis, etc. is difficult to be raised.
Cloudy peritoneal fluid is usually seen and examination of the peritoneal fluid can reveal an increased white blood cell count and changes similar to those seen in primary peritonitis but the "lavage effect" usually precludes other laboratory test.
Abdominal ultrasound and CT scan are useful in evaluating abdominal pain. However, these studies are commonly unrevealing in the early acute abdomen. Moreover, the presence of peritoneal free fluid in patients with CAPD is common and this finding is of poor help.
Bacteria are rarely seen on Gram stained smears but culture of peritoneal fluid usually reveals a single organism or less commonly, a polymicrobial enteric infection. In any case, several days are required to obtain positive multiple enteric organisms cultures and raise the suspicion of gastrointestinal disease.
In summary, the general diagnosis of peritonitis in patients with CAPD is not a difficult issue but early isolation of those patients with polymicrobial peritonitis from gastrointestinal source is difficult. The presentation and course of common gastrointestinal disease such as acute appendicitis seem to be atypical in patients undergoing CAPD. Thus, the management of these patients remains as a challenging experience for both surgeons and nephrologists.
SURGICAL MANAGEMENT
Most patients with symptoms of peritonitis are more likely to have a primary peritonitis related to the use of CAPD catheters. Catheter related peritonitis in CAPD patients are treated with a protocol of intraperitoneal antibiotics until complete resolution of symptoms. In this context, patients are first treated with antibiotics and this fact, invariably adds to the delay in diagnosis and definitive treatment if a gastrointestinal origin is present. Delay in diagnosis and definitive treatment of acute abdomen in patients undergoing CAPD is related with an extremely high mortality rate (50%) – Am Surg 2001, 67: 615-618).
The effect of the intraperitoneal antibiotic lavage on a primary inflammatory focus is unclear and it is likely that it allows for partial treatment of appendicitis, cholecystitis, diverticulitis and other diseases without gross fecal contamination.
Surgical exploration is a challenging decision because preoperative diagnosis is difficult and postoperative adhesions can preclude CAPD. At this point, we want to strongly draw your attention to the fact that ultrasound exploration and CT scan are less sensitive for detecting abdominal process because of the presence of peritoneal fluid. It is our opinion and our experience with acute abdomen in the general population that negative imaging studies never exclude an abdominal severe disease. In our experience, delay in diagnosis and treatment of acute abdomen in high-risk patients invariably increases morbidity and mortality rates and early surgical approach is preferred.
In terms of timing, we have found that the earliest surgery offers the best chance of success.
A liberal policy of surgical exploration is not probably advisable in all these patients because of the common presence of primary peritonitis not related with gastrointestinal diseases.
Patients that worsen or fail to resolve with correct intraperitoneal and systemic antibiotic therapy and those with suspicious imaging test can benefit of a more aggressive approach and surgical exploration should be performed.
LAPAROTOMY OR LAPAROSCOPY
The laparoscopic approach in patients with acute abdomen is feasible and safe in experienced hands. Laparoscopy is the only minimally invasive approach that provides diagnostic accuracy as well as therapeutic capabilities.
Laparoscopy reduces intraperitoneal adhesions, reduces postoperative pain, improves recovery of gastrointestinal function, reduces hospitalisation and health care costs and improves cosmetics results.
In our experience, diagnostic laparoscopy without findings (we always performed appendectomy) in patients with acute abdominal pain is related with a minimal morbidity rate with poor clinical significance (wound infection) that are clearly exceeded by the prognosis of the acute abdomen with a delayed treatment.
Last but not least, we consider the surgeon’s experience to be crucial. We must to offer the same opportunity for cure to the patients whether they are undergoing CAPD or not and whether they are treated with laparoscopy or an open technique. For this reason, in our opinion, early laparoscopic exploration is advisable in patients with acute abdomen undergoing CAPD but it should be performed only when well-trained surgeons are on-call.
Finally, we want you to enjoy taking a view of our surgery. All of the following pictures have been taken in the emergency surgical room at the Hospital General "La Mancha-Centro", Alcázar de San Juan, Ciudad Real, Spain.
For further information you will be welcome at our web site (LAPAROSCOPIA ON LINE) that is highly recommended. If you are interested, you will find images, video-clips and complete videos about acute abdomen and we will be very glad to discuss about them. The following images are only an example. More material makes this document too heavy to be downloaded from the internet.
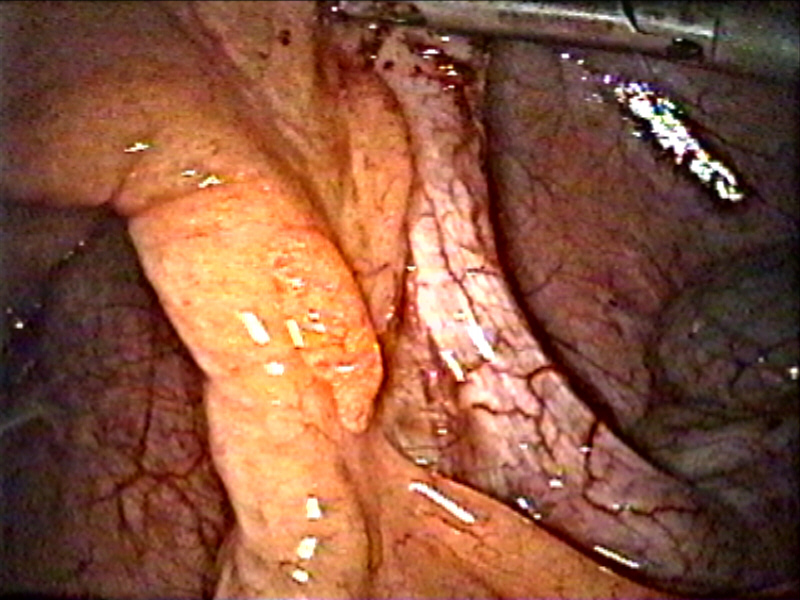

Perforated duodenal ulcer.
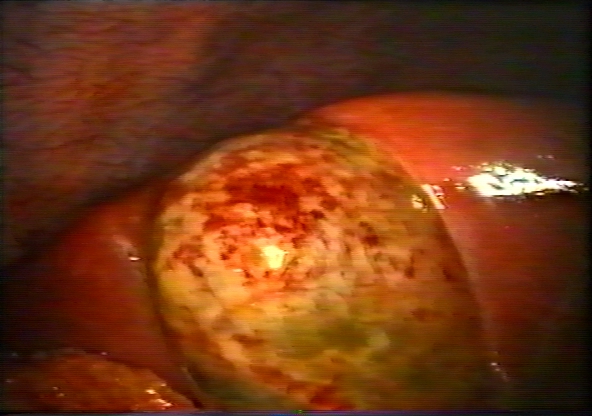
Acute cholecystitis.