
 |
|
|
Methods: Adult critically ill patients were randomized if they were oliguric (<1 ml/kg/h) with a creatinine clearance (Ccr) < 60 mL/min., and septic (>1 sepsis criterium) to receive either low-dose dopamine, torsemide, low-dose dopamine plus torsemide, or conventional therapy. Hemodynamic optimization (blood pressure and filling pressures) had to be achieved at baseline and maintained during the protocol. Ccr and other renal and systemic variables were determined baseline and at 12, 24, 48, 96 hours, and 7 days. Analysis was done by intention to treat. Results: 74 patients were studied. 32 had Ccr > 60 ml/min and were not included, and 42 were randomized to dopamine (DA) (n=12), torsemide (TOR) (n=10), dopamine plus torsemide (DA+TOR) (n=10), and control group (C) (n=10). Baseline demographics and renal function at inclusion were comparable between groups with a median urine output at inclusion of 23.4 (IQR 15; 32.6) ml/h. and a median Ccr of 19.6 (IQR 10.9; 42.2) ml/min. During the 1st hour median diuresis was 25.5 ml/h (25; 30.6) in C, 32.5 (14; 83.7) with DA, 115 (14.2; 380) with TOR, and 110 (52.5; 250) with DA+TOR (p=0.02). No significant differences of Ccr between groups were detected at any time point. The incidence of ARF, the need for CRRT, and ICU-mortality were similar in all groups. Conclusions: Neither low-dose dopamine nor a loop diuretic prevent renal failure or the need for CRRT in oliguric patients with sepsis. Methods The primary outcome measure for the study was acute renal failure or the need for renal replacement therapy (RRT). Patients Between July 1998 and January 2001, we screened all patients admitted to our general ICU for the presence of
Oliguria was defined as a urine-output below 1 ml/kg/h on two consecutive hours and it had to persist in spite of adequate hemodynamic resuscitation (Figure 1): The use of crystalloid and/or colloid solutions and norepinephrine and dobutamine infusions and their respective dosing were left to the decision of the attending physician. Dopamine infusions for hemodynamic optimization were not allowed. After volume resuscitation, the patients were included if urine output remained < 1 ml/kg/h and a two-hour creatinine clearance was lower than 60 ml/min. Additional inclusion criteria were the presence of an indwelling urinary catheter, a central venous catheter and a serum creatinine within normal range in the previous 48 hours. Hemodynamic goals had to be maintained from inclusion till day 7 (the end of the protocol). Exclusion criteria were: presence of acute renal parenchyma disease, urinary tract obstruction (ruled out by ultrasound), pregnancy, age under 18 years; chronic renal failure; cirrhosis, significant fluid overload requiring diuretic therapy (i.e. acute pulmonary edema), known allergy to study drugs, and patients with refractory septic shock, in whom filling pressures and systemic blood pressure could not be raised to 12 and 70 mmHg, respectively. Permission to proceed with the trial was obtained from the institutional ethics committee. Patients or their next of kin gave informed consent to participate in the trial. Design and Protocol The patients were randomly assigned (closed envelope) to four study groups in blocks of sixteen. Study Groups were: low-dose dopamine, torsemide, low-dose dopamine with torsemide, and a control group. Low-dose dopamine was infused at 2 m g kg-1 min-1 for 7 days or until discharge from the ICU or until side effects occurred. IV boluses of torsemide were given whenever diuresis dropped below 1 ml/kg/h and to maintain a urine output of 1-2 ml/kg/h (table 1). Measurements Measurements were performed baseline and at 12, 24, 48, 96 hours, and 7 days after inclusion: hemodynamic parameters, plasma and urine electrolytes, renal variables, and vasoactive drug doses. We recorded each patient’s baseline characteristics, Apache II score at ICU admission and at inclusion and Marshall’s MODS score at inclusion and on day 7. Patients were followed till ICU and hospital discharge. Acute renal failure was defined as a serum creatinine increase of more than 0.5 mg/dL per day on three consecutive days (41 m mol/L/day). Pre-defined indications to institute RRT are listed in table 2. Secondary outcome measures were urine output, fluid balance, natriuresis, length of ICU stay, ICU-mortality, adverse events (electrolytic abnormalities, arrhythmias, ototoxicity, associated with CRRTs), and long-term renal function (last plasma creatinine concentration available, during hospital stay or clinic visits). An audiometric test was performed one month after ICU discharge. Patients with oliguria but Ccr ³ 60 ml/min. were followed for occurrence of renal failure or need for CRRT. Results We studied 74 patients over 30 months: Of the 42 included patients (35 + 7), 10 were allocated to the control group, 12 to the dopamine group, 10 to the torsemide group, and 10 to the torsemide and dopamine group. In 4 patients protocol violations occurred: Baseline characteristics (age, sex, severity scores, underlying diseases, risk factors for chronic renal disease and ARF, haemodynamic and renal variables) are listed in table 3 and were similar between groups. Median number of sepsis criteria at inclusion was 3 (2.75, 4). The patients required a median of 19 hours (9, 31.5) of fluid resuscitation and administration of vasoactive amines with a median positive fluid balance in the previous 24 hours of 3387 (2021, 4371) ml in order to reach hemodynamic goals. Median duration of oliguria prior to inclusion was 23 hours (13.75, 32.25). Renal function at inclusion was comparable between groups (table 3) with a median urine output of 23.4 ml/h (IQR 15; 32.6) and a median Ccr of 19.6 ml/ min (IQR 10.9; 42.2). Urine output of the first hour after inclusion increased significantly in those receiving torsemide and torsemide with dopamine (p=0.028) (table 4), with an important rise. There was no significant correlation between prior urine output or baseline Ccr and diuretic response of the first hour. Fractional excretion of sodium at 12 hours also was significantly higher in the torsemide and torsemide – dopamine groups (p=0.008) (table 4). No significant differences of Ccr between groups were detected at any time point (table 4). The global combined clinical endpoint of the incidence of ARF (23 patients, 54.8%) and/or need for RRT (14 patients, 33.3%) was 23 patients (54.8%)(table 4), with no significant differences between study groups, as was the respective incidence of oliguric / non-oliguric ARF. There were also no differences in length of ICU-stay, ICU-mortality, and hospital mortality (table 4). The incidence of adverse events was not statistically different between study groups. Supraventricular tachycardia occurred most frequently in patients receiving torsemide with dopamine (5, 50%) (table 4), and required stopping of dopamine infusion in 1 patient, in whom there was an evident temporal association. Two patients in the control group (20%), 2 receiving dopamine (16.7%), and 1 receiving torsemide (10%) had at least 1 episode of supraventricular tachycardia. A similar proportion of patients received nephrotoxic drugs during the protocol (Vancomycin, aminoglycosides, angiotensin-converting-enzyme inhibitors, radiocontrast agents, and amphotericin B), or had hyperbilirrubinemia. The 39 septic oliguric patients who were not included because of baseline Ccr > 60 ml/min, had a median Ccr of 97.5 (IQR 73.5, 116.25) ml/min. ARF occurred in 3 patients (7.7%) in this group, all of whom required RRTs, while all the other 36 (92.3%) patients increased their urine output and Ccr over time without requiring further interventions. Figure 1. Flow-diagram at inclusion. 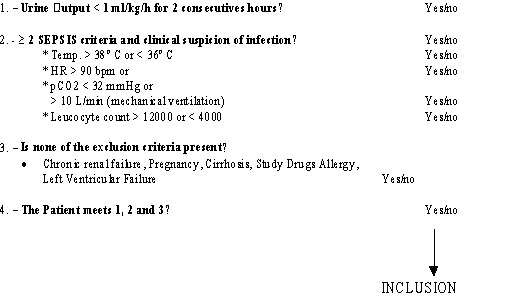
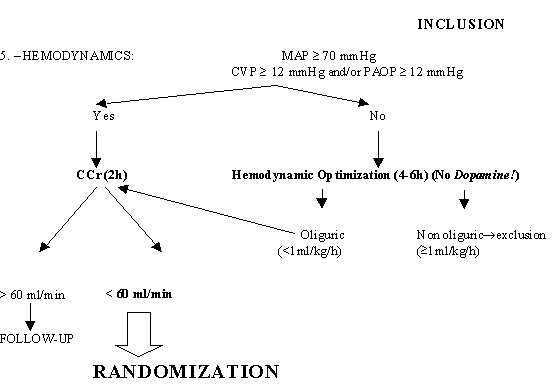
Table 1. Torsemide dosing schedule.
* Baseline Creatinine clearance (mL/min). Table 2.
Table 3. Baseline characteristics.
* Median (IQR). Mean ± SD. MODS (Multi-Organ Dysfunction Syndrome) PCr (plasma creatinine), CCr (creatinine clearance) MAP (Medium arterial Pressure), CVP (Central Venous Pressure) CO (Cardiac Output). Table 4. Results.
All comparisons between groups not statistically significant (p>0.05), except UO +1h, UNa 12h, and FENa 12h. Correspondence:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||