Introduction
Malignant hypertension (MHT) defined as severe hypertension with retinal exudates and haemorrhages with or without papilloedema [1] is an important cause of morbidity in underserved communities [2, 3] and elsewhere [4,5]. Essential hypertension remains the commonest cause [2-4], but a greater proportion of cases of secondary hypertension occurs in MHT than in benign hypertension. Morbidity from MHT is significantly worse than in BHT largely because of the renal complications [6], but the involvement of the kidneys is variable. Reports suggest that there are different course and severity of MHT in various ethnic groups with the worst outcomes occurring in Blacks [7,8] and, indeed, it has been reported to be commonest cause of end-stage renal disease in Blacks in South Africa [9]. This account focuses on the involvement of the kidneys in MHT, and with particular regard to the picture in Blacks.
Pathology of the kidneys
Underlying renal disease may confound the features of renal involvement in MHT, but in cases of primary or essential MHT the picture is more clearly differentiated. With the naked eye, the kidneys are coarsely granular and the petechial haemorrhages, which give them the flea-bitten appearance, are often visible.
The mucoid intimal proliferation (MIP), seen in the interlobular artery (Figure 1) and afferent arteriole, and fibrinoid necrosis (Figure 2), seen in the interlobular artery, afferent arteriole and glomerular tufts, are the characteristic histological findings [10, 11] and have been found to correlate with renal dysfunction in different reports.
 Figure 1.- Mucoid intimal proliferation in an interlobular artery. Jones' silver x400. Reproduced from ref. 12
Figure 1.- Mucoid intimal proliferation in an interlobular artery. Jones' silver x400. Reproduced from ref. 12
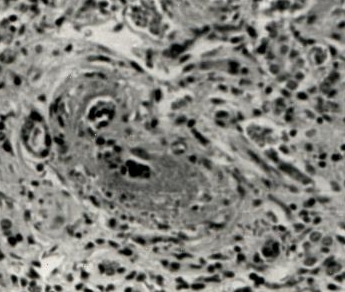 Figure 2. Fibrinoid necrosis . Haematoxylin & eosin x160. Reproduced from ref. 12
Figure 2. Fibrinoid necrosis . Haematoxylin & eosin x160. Reproduced from ref. 12
The MIP is basically occlusive while the FN is destructive. Their relative frequencies vary; some reports suggest that MIP is the more characteristic lesion [11,12], and some others restate this but only with regard to Blacks [13]. In Ibadan, Nigeria [12], but not in South Africa [14], MIP was found in all kidney sections in studies of MHT. The absence of fibrinoid necrosis from some sections has sometimes been attributed to a sampling error in biopsy specimens and a possible relationship to terminal uraemia. Another report from Ibadan describes the occurrence of various stages of focal and segmental glomerulosclerosis (FSG) in essential MHT and suggests that FSG, in addition to the MIP and FN, may contribute to the renal dysfunction seen in MHT [15]. It is notable however, that FSG is generally commoner in Blacks [16] and may therefore represent a non-specific response to injury in these patients.
Other relevant findings in MHT include thickening and wrinkling of glomerular capillary walls and contracted glomerular beds, prominent juxta-glomerular apparatus [17], glomerular epithelial cell droplets [18], and thickening and wrinkling of tubular basement membrane. Correlations have been shown between the tubular changes and renal function [12] and between the vascular lesions and plasma renin activity (PRA) and also between the vascular lesions and the epithelial cell droplets [18].
Clinical features
The clinical picture is similarly variable. Oliguria, proteinuria, haematuria and renal failure are common [2,3] and indeed, in a study in Ibadan, proteinuria (generally non-nephrotic in essential MHT) and microscopic haematuria were present in 100% of cases, oliguria in 52% and renal failure in 77% at Presentation [2]. This contrasts with the picture in Birmingham, Great Britain, where up to 60% of cases had no complications and only 31.7% presented with chronic renal failure [4], in White South Africans in whom MHT rarely occurred [3], and in Italy where the complications appeared to have diminished over the years [19].
Owing to the severe intra-renal ischaemia, plasma rennin levels are generally elevated. Renal function, as measured by serum creatinine, may be normal or the patients may present with acute, chronic or acute on chronic renal failure. In Ibadan, we found serum creatinine to be negatively correlated with mean arterial pressure at presentation [20] (Figure 3), and rose with lowering of the BP, implying that in untreated patients, the renal function was, perhaps, maintained by the BP in the short term. This contrasted with a later report from Italy [19] in which the glomerular filtration rate was negatively correlated with diastolic BP at presentation but in both reports however, control of BP lead to an early, and often transient, worsening of renal function.
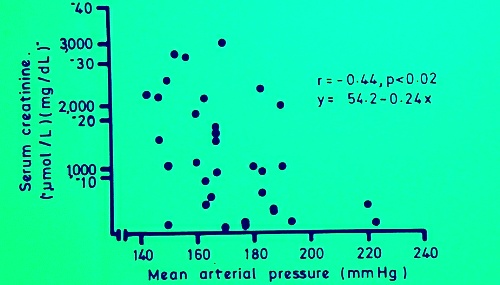 Figure 3. Relationship between mean arterial pressure and serum creatinine at presentation.
Figure 3. Relationship between mean arterial pressure and serum creatinine at presentation. Acute renal failure results from the occlusive and necrotic arteriolar and glomerular lesions, and from acute tubular necrosis consequent upon intra-renal ischaemia. Complete recovery from this stage is possible with adequate control of BP and provision of dialysis [3]. Patients who recover are likely to have had a short history of MHT with rapidly rising BP and oligo-anuria.
In patients who present with chronic renal failure or develop chronic renal failure afterwards, the course may be influenced by several factors. In our series [20], patients with initial serum creatinine >3.6mg/dL had a rise of serum creatinine that generally necessitated dialysis following the lowering of BP, in contrast to those with serum creatinine <3.2md/dL who generally did not require early dialysis. This has also been reported in other studies with only slightly differing serum creatinine levels and time frames [19,21]. Long-term control of BP is essential even after a rise in serum creatinine level follows the reduction of BP, but dialysis may be required in a substantial proportion of cases. In some, renal function recovers sufficiently to allow for withdrawal of dialysis [21,22], and in this regard, up to 6 or 12 months of dialysis must be allowed before decisions are made about renal transplantation.
Choice of therapy.
As with other cases of hypertension, reduction of BP is paramount [24], but there are reports that suggest the indication for the use of certain agents. Good results, by way of BP control and preservation of renal function, have been obtained from the use of beta-blockers, calcium antagonists [25, 26] and angiotensin converting enzyme inhibitors, and in rats, angiotensin receptor blockers have been shown to prevent the development of malignant vascular injury independently of the effect on BP [27]. The use of dihydropyridine calcium antagonists in renal failure with proteinuria should perhaps be re-evaluated in the light of the AASK study in which a worsening of proteinuria and progression of renal disease was found in Black patients [28].
Very tight control of BP should perhaps be avoided in the first few days and a DBP of 90-110mm Hg is usually aimed for [3]. According to current recommendations, long term BP control should be to below 135/85 mmHg [29], but even when the BP control has been sub-optimal some preservation of renal function appears to have been possible [19].
Patients who require dialysis benefit from both haemodialysis and peritoneal dialysis. The outlook on haemodialysis is no different from that of other patients with other causes of chronic renal failure [3,30]. Chronic ambulatory peritoneal dialysis should be used in appropriate patients, and there is a report that this mode of therapy may be better than haemodialysis in some patients with MHT [31].
Outcome.
The outcome in MHT remains poor in many Blacks in Africa and the United States. One-year survival in our previous report was 37.5% [2], although some patients had been lost to follow-up, but the picture in South Africa in the eighties was somewhat better with a 1-year survival of 75% [3]. There are indications that higher BP at presentation, oliguria, and less significantly, renal function at presentation and female gender may be predictive of renal recovery in Black South Africans [23]. Compared to Whites, the poor outcome in Blacks with MHT may be related to the poorer renal function at presentation [8], severer course of renal disease in Blacks and the poorer availability of renal replacement therapy to these patients. With improvements in the diagnosis and treatment of non-malignant hypertension, the incidence [32] and severity of MHT [19,33] have diminished in many parts of the world, and its prognosis improved. Five-year survivals of 74% [8] and 71.9% [19] have been reported from Europe (Table 1), and in the latter report [19] survival has been 100% in cases seen after 1980.
|
Nigeria[2] |
South Africa[3] |
G. Britain[8] |
Italy[19] |
|
Renal failure at presentation |
77% |
82% |
31.7% |
|
| 1-year survival |
37.5% |
75% |
|
95% |
|
5-year survival |
|
|
74% |
79.1% |
| Factors favouring prognosis |
|
Serum creatinine <500umol/L |
Less severe renal failure |
Se-creatinine <2mg/dL. BP control. |
Table 1. Comparison of outcomes in malignant hypertension in 4 countries
The long-term outlook in MHT is favoured by lower serum creatinine at presentation [5,8], shorter duration of known hypertension [8], good BP control at follow-up [34] and, clearly, the availability of renal replacement therapy.
References
1. Ahmed MEK, Walker JM, Beevers DG, Beevers M. Lack of difference between malignant and accelerated hypertension. Br Med J 1986; 292:235-237
2. Kadiri S, Olutade BO. The clinical presentation of malignant hypertension in Nigerians. J Hum Hypertens. 1991; 5:339-343
3. Milne FN, James SH, Veriava Y. Malignant hypertension and its renal complications in black SouthAfricans. S Afr Med J 1989; 76:164-167
4. Lip GY, Beevers M, Beevers G. The failure of malignant hypertension to decline:A survey of 24 years’ experience in a multiracial population in England. J Hypertens 1994; 12:1297-1305
5.Scarpelli PT, Gallo M, De Cesaris F et al. Continuing follow-up of malignant hypertension. J Nephrol 2002; 15:431-437
6. Isles CG, Lim KG, Boulton-Jones M et al. Factors influencing mortality in malignant hypertension. J Hypertens 1985; 3 Suppl 3: S 405- S 407
7. Woods JW. Malignant hypertension: clinical recognition and management. Cardiovasc Clinics 1978; 9: 311-320
8. Lip GY, Beevers M, Beevers DG. Complications and survival of 315 patients with malignant-phase hypertension. J Hypertens 1995; 13: 915-924
9. Gold CH, Isaacson C, Levin J. The pathological basis of end-stage renal disease in blacks. S Afr Med J 1982; 61:263-265
10. Schwartz GL, Strong CG. Renal parenchymal involvement in essential hypertension Med Clin North Am 1987; 71:843-858
11. Kincaid-Smith P. Malignant hypertension 1991; 9:893-899
12. Kadiri S, Thomas JO. Kidney histology and clinical correlates in malignant hypertension. East Afr Med J 1993; 70:112-116
13. Pitcock JA, Johnson JG, Hatch FE, Acchiardo S, Muirhead FE, Brown PS. Malignant hypertension in blacks: malignant intrarenal disease as observed by light and electron microscopy. Hum Pathol 1976; 7:333-346
14. Isaacson C, Milne FJ, van Niekerk I, Kenyon MR, Mzamane DV. The renal histopathology of essential malignant hypertension in black South Africans. S Afr Med J 1991; 80:173-176
15. Kadiri S, Thomas JO. Focal segmental glomerulosclerosis in malignant hypertension. S Afr Med J 2002; 92:303-305
16. Korbet SM, Genchi RM, Borok RZ, Schwartz MM. The racial prevalence of glomerular lesions in nephrotic adults. Am J Kidney Dis 1996;27: 647-651.
17. Jones DB. Arterial and glomerular lesions associated with severe hypertension. Lab Invest 1974; 31:303-313
18. Kincaid-Smith P, Owen J, Whitworth JA, Walter MA, Doyle A, Woods RA. Glomerular and vascular changes in malignant hypertension. Clin Exp Hypertens 1984; A6: 471-491
19. Scarpelli PT, Livi R, caselli G et al. Accelerated (malignant) hypertension: a study of 121 cases between 1974 and 1996. J Nephrol 1997; 10: 207-215
20. Kadiri S, Olutade BO. Short term course of renal function in accelerated hypertension. Afr J Med med Sci 1993; 22: 25-29
21. Lawton WJ. The short-term course of renal function in malignant hypertensives with renal insufficiency. Clin Nephrol 1982; 17: 277-283
22. Yaqoob M, McClelland P, Ahmad R. Delayed recovery of renal function in patients with acute renal failure due to accelerated hypertension. Postgrad Med J 1991; 67: 829-831
23. James SH, Meyers AM, Milne FJ, Reinach SG. Partial recovery of renal function in black patients with apparent end-stage renal failure due to primary malignant hypertension. Nephron 1995; 71: 29-34
24. Ruggenenti P, Schieppati A, Remuzzi G. Progression, remission, regression of chronic renal diseases. Ancet 2001; 357: 1601-1608
25. IslesCG, Johnson AOC, Milne FJ. Slow-release nifedipine and atenolol in initial treatment in blacks with malignant hypertension. Br J Pharmacol 1986; 21: 377-383.
26. Suzuki H, Nakamoto H, Nemoto H, Sugahara S, Okada H. Control of blood pressure and preventionof end-organ damage in patients with accelerated hypertension by combination with arotinolol and extended release nifedipne. Hypertens Res 2000; 23: 159-166
27. Hilgers KF, Hartner A, Porst M, Veelken R, Mann JF. Angiotensin II type receptor blockade prevents lethal malignant hypertension: relation to kidney inflammation. Circulation 2001; 104: 1436-1440
28. Wright JT, Bakris G, Greene T et al. for the African American Study of Kidney Disease and Hypertension Study Group. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease. Results from the AASK trial. JAMA 2002; 288: 2421-2431
29. Peterson JC, Adler S, Burkart JM et al. Blood pressure control, proteinuria, and the progression of renal disease: the Modification of Diet in Renal Disease study. Ann Intern Med;1995; 123: 754-762.
30. De Lima JJ, da Fonseca JA, Godoy A, Bortolotto LA, Krieger EM. Outcome of patients with malignant hypertension and end-stage renal failure treated by long-term haemodialysis. Cardiology 1999; 92: 93-98
31. Katz IJ, Sofianou L, Butler O, Hopley M. Recovery of renal function in Black South African patients with malignant hypertension: superiority of continuous ambulatory peritoneal dialysis over haemodialysis. Perit Dial Int 2001; 21: 581-586
32. Perry HM, Freis ED, Frohlich ED. Department of Veterans Affairs hypertension meeting: a proposal for improved care. Hypertension 2000; 35: 853-857
33. Ohta Y, Tsuchihashi T, Ohya Y et al. Trends in the pathophysiological characteristics of malignant hypertension. Hypertens Res 2001; 24: 489-492
34. Lip GYH, Beevers M, Beevers DG. Does renal function improve after diagnosis of malignant-phase hypertension? J Hypertens 1997; 15: 1309-1315.
