Some epidemiological studies on blood pressure
among children and adolescents have revealed
that blood pressure levels in childhood
are the strongest predictors of adult blood pressure
levels. In the adult population, hypertension
causes a two to threefold increase in an
individual's risk of cardiovascular morbidity. Cardiovascular
risk depends on blood pressure itself,
coexistent risk factors and whether there is
hypertensive end-organ damage. Therefore,
accuracy in determining blood pressure is essential
and a standardized protocol should be
considered for blood pressure measurement,
which would make the comparison of results
obtained by different studies in different countries
possible. This article reviews the main determinants
of accuracy for casual and ambulatory
blood pressure measurements in children.
KEY WORDS
Blood. Pressure. Methodology. Children.
Adolescent.
INTRODUCTION
Cardiovascular diseases are the main
causes of death in Brazil. Stroke mortality rates
among Brazilians are high, reflecting the burden
of hypertension. Some international epidemiological
studies on blood pressure among
children and adolescents have revealed that
blood pressure levels in childhood are the
strongest predictor of adult blood pressure levels
1-3. In the adult population, hypertension
causes a two to threefold increase in an individual's
risk of cardiovascular morbidity4,5. The
relationship between hypertension and cardiovascular
disease seems to be continuous: cardiovascular
risk depends on blood pressure
itself, coexistent risk factors and whether there
is hypertensive end-organ damage.
As accuracy in determining blood pressure
is essential, a standardized protocol
should be considered for blood pressure
measurement, which would make the comparison
of results obtained by different studies
in different countries possible. Observers
should be trained and certified to minimize
measurement bias. Homogeneous decisions
should be taken regarding equipment factors
such as an appropriate cuff bladder size or
the alternative use of mercury manometers
or oscillometric devices. Technical factors
such as the recording of fourth, fifth or both
Korotkoff sounds for diastolic blood pressure
need to be taken into consideration. Also,
the number of measurements needed for estimating
a child's blood pressure and the influence
on its measured value of environmental
factors such as the time of the day and
ambient temperature must be considered6.
Some of these factors will be discussed separately
in the next paragraphs.
The cuff
Classically, to obtain an accurate blood
pressure measurement, a cuff bladder width
of approximately 40% of the upper arm circumference
should be chosen because it most
closely approximates intra-arterial readings7.
The bladder length should be at least 90% of
arm circumference to avoid overestimation of
blood pressure, especially in children8. Another
less known effect of the cuff size change occurs
when, in accordance with the
abovementioned instructions for cuff selection,
the cuff size is changed to a larger one.
In this case, the cuff change leads to an abrupt
fall in the value of measured blood pressure
that is not arm-dependent, but cuff-dependent 9.
This very inconvenient effect may be responsible
for two issues: 1. Any association
between blood pressure and arm circumference,
such as body mass, will be biased towards
zero. 2. In longitudinal studies, when
changing to a larger cuff, measured blood pressure
is lower than previous readings, which
could lead to inappropriate inverse correlations
of blood pressure with chronological age or
height. In 1999, Arafat and Mattoo 10 reviewed
commercially available blood pressure cuffs
and detected that the sizes of available cuffs,
labeled as infant, pediatric, small adult, adult
and large adult were heterogeneous among the
different manufacturers. These authors concluded
that cuff sizes need to be standardized
and indicate bladder size, and suggested that
they should be color-coded for convenience.
Number of measurements needed
Another important issue to consider is the
number of measurements that should be repeated within a visit and between visits in order
to determine a child's blood pressure. The
work by Gillman and Cook (1993)6 demonstrated
that it depends on the instrument and
technique. For auscultatory equipment, using
a mercury manometer or random zero manometer,
among 162 children aged 8 to 12
years, the systolic blood pressure values obtained
after four weekly visits with three measurements
per visit leveled off after about 2-3
measurements per visit, but the difference
between visits was large until about the third
or fourth visit. For oscillometric equipment,
using the Dinamap model 845XT, among 106
children aged 9 to 13 years, the systolic blood
pressure values obtained after three weekly
visits with four measurements per visit demonstrated
that for the Dinamap device the first
of several measurements during one particular
visit was generally higher than the following
ones. The values obtained started to level
off after 4-5 measurements within a visit, with
the "first measurement effect" reproducible
even after 3 consecutive visits.
The diastolic dilemma
There has been an ongoing controversy
over whether the muffling (Korotkoff 4-
K4) or disappearance of sounds (Korotkoff
5- K5) should be preferentially considered
for the measurement of diastolic blood pressure
in children11. Neither value correctly
defines intra-arterial diastolic blood pressure,
since K5 is approximately 9 mmHg
higher than direct diastolic blood pressure
and K5 is easier for the human ear to discern
than K4 12 . Current recommendations
therefore favor the use of K5.
The stethoscope diaphragm versus the bell
The bell is preferred for blood pressure
auscultation in adults. This issue is still controversial
in children, since placing the bell adequately
in small children may compress the
artery and produce falsely low diastolic values.
Thus, some authors advocate the use of the
diaphragm for small children13, while others
suggest that the bell, when properly used,
should accomplish better auscultatory results 11.
Time of the day and ambient temperature
It is clear from ambulatory blood pressure
studies that blood pressure varies over the
24 hours of the day, presenting lower values
during sleep and higher values during wakefulness,
with a peak in the morning and another
in late afternoon14. There is a negative
relationship between blood pressure and temperature.
An increase of 10°C leads to a fall of
approximately 5-7 mmHg in systolic and in
diastolic blood pressure15,16.
Do we have normative blood
pressure data for children?
Unfortunately we don't have normative
blood pressure data for the pediatric population.
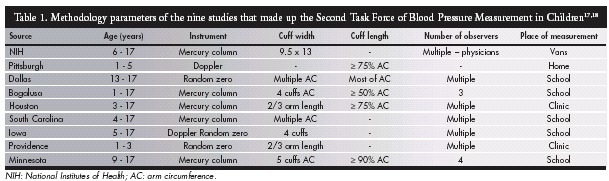
Table 1 shows the lack of homogeneous
methodology in nine studies that made
up the Second Task Force of Blood Pressure
Measurement in Children, reviewed by
Rosner et al. in 199317,18. The Update of the
Second Task Force of Blood Pressure Measurement
in Children added a tenth study to
this list (National Health and Nutrition Examination
Survey . NHANES III)19.
Table
2 shows the same lack of methodological
homogeneity in the six studies from which
the European pediatric blood pressure normative
data is at present derived20.
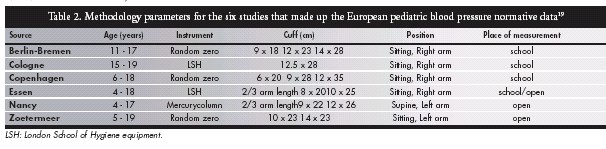
It is important to emphasize that this lack
of homogeneity is not a consequence of carelessness
but rather of the multiple difficulties
involved in performing epidemiological studies
in the pediatric age group. Unfortunately,
according to Nielsen et al. (1989)21 , "confusion
concerning the most suitable cuff ... is
responsible for at least some of the scatter between
blood pressure studies". Arafat and
Mattoo (1999) 10, referring to the Update of
the Second Task Force of Blood Pressure Measurement
in Children, suggested that "a new
multicenter study, using uniform criteria for
cuff selection, may be necessary to establish
the accuracy of the published nomogram on
normal blood pressure in children".
What blood pressure measuring
device should be used in the future?
The mercury manometer is our old friend.
It is simple, accurate and easy to service. Standard
Hg readings are the main basis for blood
pressure-disease associations and,
blood pressure readings with this instrument
are subject to terminal digit preference and
observer bias, observer training could possibly
eliminate this problem. Unfortunately,
mercury has toxic effects on the environment
and the mercury manometer will have to be
gradually replaced.
The aneroid sphygmomanometer registers
blood pressure through a mechanically intricate
system. Its accuracy is affected by everyday
use. When calibrated against a mercury
manometer a mean difference of 3 mmHg is
acceptable, although up to 30% have errors of
more than 7 mmHg. Readings are also subject
to terminal digit preference and observer bias22 .
What about automated sphygmomanometry?
The most widely used oscillometric devices
are manufactured under the name
"Dinamap". Several models have been developed,
each with an updated algorithm. Validation
data has to be obtained separately for
each model. Systolic and diastolic blood pressures
are calculated as a function of the mean
arterial pressure, which is the point of maximal
oscillation and are calibrated to be equivalent
to intra-aortic pressures. The devices are
easy to use and strongly correlated to intra-arterial
readings. Accuracy is affected by arm
movement and measurements are affected by
the "first-reading effect"23.
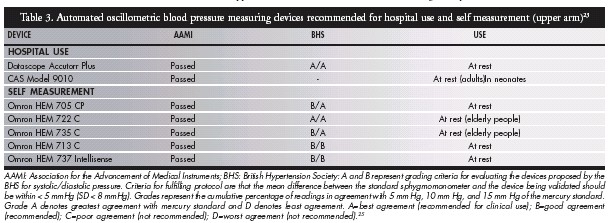
Automated oscillometric devices have to
be validated before they can be recommended
for clinical use. Validation protocols based
on comparative measurements between oscillometric
equipment and the mercury manometer
were devised by the British Hypertension
Society and the American Association
of Medical Instruments24. The two
protocols have now been reconciled and are
used in association to validate oscillometric
devices. Table 3 presents the instruments
currently validated and recommended for
hospital use and self-measurement (home
blood pressure)25,26.
Is it possible to use auscultatory and oscillometric
devices interchangeably? Unfortunately
not, as Korotkoff is approximately 3
mmHg lower than direct systolic blood pressure
and, as we mentioned earlier, K5 is approximately
9 mmHg higher than direct
diastolic blood pressure 12 . Park et al.
(2001)27 tested the Dinamap 8100 against the
standard mercury manometer and found that
the equipment detected mean systolic and
diastolic blood pressure values significantly
above auscultatory readings. On the other
hand, Barker et al. (2000) 28 tested the Omron
M1 against the standard mercury manometer
and concluded that the Omron M1 overestimates
higher pressures and underestimates
lower pressures. There is a lack of validated
and approved automated devices for use in
clinical and epidemiological setting for the
pediatric age group 29.
Ambulatory blood pressure
monitoring in children
The current general indications for ambulatory
blood pressure monitoring are: identification
of white coat hypertension, borderline
hypertension, identification of nocturnal hypertension,
drug resistant hypertension, indication
of antihypertensive medication, hypertension
of pregnancy and identification of hypotension30.
Among the current issues for ambulatory
blood pressure monitoring use in
pediatrics, the main problem is the lack of definite
normative data. The methodology is promising,
since recordings show good accuracy and
reproducibility in children31. Up-to-date definitions
of sleep/wake periods, using actigraphy
or a detailed diary of daily activities, are necessary
for accurately determining the sleep blood
pressure decline 32. The white coat effect (white
coat hypertension or white coat normotension)
known within the literature relating to adults
has also been confirmed in the pediatric population.
In the same way as for adults, the left
ventricular mass index and left ventricular
hypertrophy are more closely related in children
to 24-hour systolic blood pressure than
with casual systolic blood pressure 33. According
to Kapuku et al. (1999) 34 left ventricular
hypertrophy can be predicted by initial ambulatory
systolic parameters.
In a recent study 35, our group compared
casual blood pressure and ambulatory blood
pressure monitoring parameters among normotensive
and hypertensive adolescents.
Casual blood pressure was measured by two
trained observers in two different and separate
environments (clinic and ambulatory
blood pressure monitoring unit). For systolic
and diastolic blood pressure, in both normotensive
and hypertensive populations, an
alarm reaction was demonstrated during exposure
to an unknown environment and
observer (the ambulatory blood pressure
monitoring unit). It should also be noted
that, contrary to findings in adult
populations, the mean casual systolic/
diastolic blood pressure measured in the
clinic was lower than the mean ambulatory
blood pressure monitoring parameters while
awake, for normotensive and hypertensive
adolescents. The same study compared findings
from casual auscultatory measurements
(in the clinic and ambulatory blood pressure
monitoring unit) and ambulatory blood pressure monitoring parameters among hypertensive
adolescents. The parameters included
systolic and diastolic ambulatory blood pressure
monitoring methods, systolic and
diastolic blood pressure descent during sleep
(systolic/diastolic sleep blood pressure descent),
systolic and diastolic blood pressure
load. This led us to conclude that, although
normality parameters are still under development
for ambulatory blood pressure monitoring
in the pediatric age range, ambulatory
blood pressure monitoring is a promising tool
for the follow-up of pediatric hypertensive
patients. In this respect it seems superior to
casual blood pressure evaluation, since it uncovers
the white coat effect.
Ambulatory blood pressure monitoring
device validation data for children is scarce.
The Spacelabs 90207, widely used in pediatric
studies, and the TM 2421, used in a recent
large pediatric study 36 are equipment that has
not scored well enough to be recommended
according to the protocols of the British Hypertension
Society and the American Association
of Medical Instruments. At present, the
only device recommended for children, according to these protocols, is the QuietTrak 37.
Amazingly, this is a piece of auscultatory
equipment, a type of device generally not
adopted in pediatric studies because the noise
of children in movement interferes with the
accuracy of the microphone determination of
the measured blood pressure value.
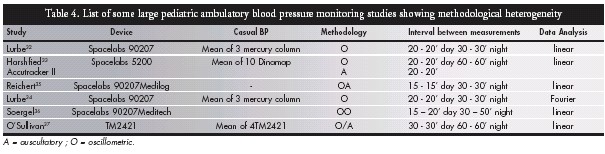
Table 4
shows a list of some large pediatric ambulatory
blood pressure monitoring studies 36,38-42
and demonstrates that, as for casual blood
pressure, studies are being performed without
methodological homogeneity. Different
devices, with different measurement protocols,
cannot be considered together to generate
norms.
In conclusion, as of today, the main problem
for the diagnosis and management of hypertension
in children is the lack of good normative
data for casual and ambulatory blood
pressure values. The only solution for this issue
is to propose a multicenter study with a
homogenous protocol, in order to obtain normal
multiethnic casual and ambulatory
pediatric blood pressure values. Only then will
studies to correlate blood pressure level and
hypertensive end-organ damage be possible.
REFERENCES
1. Lauer RM, Clarke WR. Childhood risk factors for high adult blood
pressure: the Muscatine Study. Pediatrics 1989;84(4):633-41.
2. Hoq S, Chen W, Srinivasan SR, Berenson GS. Childhood blood
pressure predicts adult microalbuminuria in African Americans,
but not in whites: the Bogalusa heart study. Am J Hypertens
2002;15(12):1036-41.
3. Gillman MW, Ellison RC. Childhood prevention of essential
hypertension. Pediatr Clin North Am 1993;40(1):179-94.
4. Kannel WB. Blood pressure as a cardiovascular risk factor: prevention
and treatment. JAMA 1996;275(20):1571-6.
5. Klag MJ, Whelton PK, Randall BL. Blood pressure and end-stage
renal disease in men. N Engl J Med 1996;334(1):13-8.
6. Gillman MW, Cook NR. Blood pressure measurement in childhood
epidemiological studies. Circulation 1995;92(4):1049-57.
7. Perloff D, Grim C, Flack J, et al. Human blood pressure determination
by sphygmomanometry. Circulation 1993;88 (5 Pt
1): 2460-70.
8. Vyse TJ. Sphygmomanometer bladder length and measurements
of blood pressure in children. Lancet 1987;1(8532):561-2.
9. Whincup PH, Cook DG, Shaper AG. Blood pressure measurement
in children: the importance of cuff bladder size. J
Hypertens 1989;7(10):845-50.
10. Arafat M, Mattoo TK. Measurement of blood pressure in children:
recommendations and perceptions on cuff selection.
Pediatrics 1999; 104(3): e30.
11. Prineas RJ, Jacobs D. Quality of Korotkoff sounds: bell vs diaphragm,
cubital fossa vs brachial artery. Prev Med
1983;12(5):715-9.
12. Stolt M, Sjönell G, Aström H, Hansson L. Factors affecting the
validity of the standard blood pressure cuff. Clin Physiol
1993;13(6):611-620.
13. Londe S. Blood pressure measurement. Pediatrics
1987;80(6):967-8.
14. Krull F, Buck T, Offner G, Brodehl J. Twenty-four hour blood
pressure monitoring in healthy children. Eur J Pediatr
1993;152(7):555-8.
15. Prineas RJ, Gillum RF, Horibe H, Hannan PJ. The Minneapolis
children's blood pressure study. Part 1: standards of measurement for
children's blood pressure. Hypertension 1980;2(4 Pt 2):I18-24.
16. Jenner DA, English DR, Vandongen R, Beilin LJ, Armstrong
BK, Dunbar D. Environmental temperature and blood pressure
in 9-year-old Australian children. J Hypertens
1987;5(6):683-6.
17. Rosner B, Prineas RJ, Loggie JM, Daniels SR. Blood pressure
nomograms for children and adolescents, by height, sex, and
age, in the United States. J Pediatr 1993;123(6):871-86.
18. Report of the Second Task Force on Blood Pressure Control in
Children - 1987. Task Force on Blood Pressure Control in Children.
National Heart, Lung and Blood Institute, Bethesda,
Maryland. Pediatrics 1987;79(1):1-25.
19. Update on the 1987 Task Force Report on High Blood Pressure
in Children and Adolescents: a working group report from the
National High Blood Pressure Education Program. National
High Blood Pressure Education Program Working Group on
Hypertension Control in Children and Adolescents. Pediatrics
1996;98(4 Pt 1):649-58.
20. de Man SA, André JL, Bachmann H, et al. Blood pressure in
childhood: pooled findings of six European studies. J Hypertens
1991;9(2):109-14.
21. Nielsen PE, Clausen LR, Olsen CA, Olsen JA. Blood pressure
measurement in childhood and adolescence. International recommendations
and normal limits of blood pressure. Scand J
Clin Lab Invest Suppl 1989;192:7-12.
22. Beevers G, Lip GY, O'Brien E. ABC of hypertension. Blood
pressure measurement. Part II - conventional sphygmomanometry:
technique of auscultatory blood pressure measurement BMJ
2001;322(7293):1043-7.
23. Park MK, Menard SM. Normative oscillometric blood pressure
values in the first 5 years in an office setting. Am J Dis
Child 1989;143(7):860-4.
24. O'Brien E, Atkins N. A comparison of the British Hypertension
Society and Association for the Advancement of Medical
Instrumentation protocols for validating blood pressure measuring
devices: can the two be reconciled? J Hypertens
1994;12(9):1089-94.
25. O'Brien E, Coats A, Owens P, et al. Use and interpretation of
ambulatory blood pressure monitoring: recommendations of
the British Hypertension Society. BMJ 2000;320:1128-34.
26. O'Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood
pressure measuring devices: recommendations of the European
Society of Hypertension. BMJ 2001;322(7285):531-6.
27. Park MK, Menard SW, Yuan C. Comparison of auscultatory
and oscillometric blood pressures. Arch Pediatr Adolesc Med
2001;155(1):50-3.
28. Barker ME, Shiell AW, Law CM. Evaluation of the Dinamap
8100 and Omron M1 blood pressure monitors for use in children.
Paediatr Perinat Epidemiol 2000;14(2):179-86.
29. Wells TG, Neaville WA, Arnold JR, Belsha CW. Evaluation of
home blood pressure monitors in children and adolescents. Am
J Med Sci 1998;315(2):110-7.
30. O’Brien E, Beevers G, Lip GY. ABC of hypertension. Blood
pressure measurement. Part III - automated sphygmomanometry:
ambulatory blood pressure measurement. BMJ
2001;322(7294):1110-4.
31. Lurbe E, Cremades B, Rodriguez C, Torro MI, Alvarez V, Redon
J. Factors related to quality of ambulatory blood pressure monitoring
in a pediatric population. Am J Hypertens 1999;12(9 Pt
1):929-33.
32. Eissa MA, Poffenbarger T, Portman RJ. Comparison of the
actigraph versus patients’ diary information in defining circadian
time periods for analyzing ambulatory blood pressure
monitoring data. Blood Press Monit 2001;6(1):21-5.
33. Belsha CW, Wells TG, McNiece KL, Seib PM, Plummer JK,
Berry PL. Influence of diurnal blood pressure variations on target
organ abnormalities in adolescents with mild essential hypertension.
Am J Hypertens 1998;11(4 Pt 1):410-7.
34. Kapuku GK, Treiber FA, Davis HC, Harshfield GA, Cook BB,
Mensah GA. Hemodynamic function at rest, during acute stress,
and in the field: predictors of cardiac structure and function 2
years later in youth. Hypertension 1999;34(5):1026-31.
35. Koch VH, Colli A, Saito MI, et al. Comparison between casual
blood pressure and ambulatory blood pressure monitoring parameters
in healthy and hypertensive adolescents. Blood Press
Monit 2000;5(5-6):281-9.
36. O’Sullivan JJ, Derrick G, Griggs P, Foxall R, Aitkin M, Wren
C. Ambulatory blood pressure in schoolchildren. Arch Dis Child
1999;80(6):529-32.
37. O’Brien E, Waeber B, Parati G, Staessen J, Myers MG.Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ 2001;322(7285):531-6.
38. Lurbe E, Redon J, Liao Y, Tacons J, Cooper RS, Alvarez V. Ambulatory blood pressure monitoring in normotensive children. J Hypertens 1994;12(12):1417-23.
39. Harshfield GA, Alpert BS, Pulliam DA, Somes GW, Wilson
DK. Ambulatory blood pressure recordings in children and adolescents. Pediatrics 1994;94(2 Pt 1):180-4.
40. Lurbe E, Thijs L, Redon J et al. Diurnal blood pressure curve in children and adolescents. J Hypertens 1996;14(1):41-6
41. Reichert H, Lindinger A, Frey O, et al. Ambulatory blood pressure monitoring in healthy schoolchildren. Pediatr Nephrol 1995;9(3):282-6.
42. Soergel M, Kirschstein M, Busch C, et al. Oscillometric twenty-four-hour ambulatory blood pressure values in healthy children and adolescents: a multicenter trial including 1141 subjects. J
Pediatr 1997;130(2):178-84.
