Return to top.
General Recommendations on Immunization
Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the American Academy of Family Physicians (AAFP). 02/06/2002
Prepared by
William L. Atkinson, M.D.1
Larry K. Pickering, M.D.2
Benjamin Schwartz, M.D.3
Bruce G. Weniger, M.D.3
John K. Iskander, M.D.3
John C. Watson, M.D.4
1Immunization Services Division
2Office of the Director
3Epidemiology and Surveillance Division
National Immunization Program
4Division of Parasitic Diseases
National Center for Infectious Diseases
The material in this report was prepared for publication by the National Immunization Program, Walter A. Orenstein, M.D., Director; and the Immunization Services Division, Lance E. Rodewald, M.D., Director.
Summary
This report is a revision of General Recommendations on Immunization and updates the 1994 statement by the Advisory Committee on Immunization Practices (ACIP) (CDC. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices [ACIP]. MMWR 1994;43[No. RR-1]:1--38). The principal changes include expansion of the discussion of vaccination spacing and timing, recommendations for vaccinations administered by an incorrect route, information regarding needle-free injection technology, vaccination of children adopted from countries outside the United States, timing of live-virus vaccination and tuberculosis screening, expansion of the discussion and tables of contraindications and precautions regarding vaccinations, and addition of a directory of immunization resources. These recommendations are not comprehensive for each vaccine. The most recent ACIP recommendations for each specific vaccine should be consulted for additional details. This report, ACIP recommendations for each vaccine, and other information regarding immunization can be accessed at CDC's National Immunization Program website at http://www.cdc.gov/nip (accessed October 11, 2001).
Introduction
This report provides technical guidance regarding common immunization concerns for health-care providers who administer vaccines to children, adolescents, and adults. Vaccine recommendations are based on characteristics of the immunobiologic product, scientific knowledge regarding the principles of active and passive immunization, the epidemiology and burden of diseases (i.e., morbidity, mortality, costs of treatment, and loss of productivity), the safety of vaccines, and the cost analysis of preventive measures as judged by public health officials and specialists in clinical and preventive medicine.
Benefits and risks are associated with using all immunobiologics. No vaccine is completely safe or 100% effective. Benefits of vaccination include partial or complete protection against the consequences of infection for the vaccinated person, as well as overall benefits to society as a whole. Benefits include protection from symptomatic illness, improved quality of life and productivity, and prevention of death. Societal benefits include creation and maintenance of herd immunity against communicable diseases, prevention of disease outbreaks, and reduction in health-care--related costs. Vaccination risks range from common, minor, and local adverse effects to rare, severe, and life-threatening conditions. Thus, recommendations for immunization practices balance scientific evidence of benefits for each person and to society against the potential costs and risks of vaccination programs.
Standards for child and adolescent immunization practices and standards for adult immunization practices (1,2) have been published to assist with implementing vaccination programs and maximizing their benefits. Any person or institution that provides vaccination services should adopt these standards to improve immunization delivery and protect children, adolescents, and adults from vaccine-preventable diseases.
To maximize the benefits of vaccination, this report provides general information regarding immunobiologics and provides practical guidelines concerning vaccine administration and technique. To minimize risk from vaccine administration, this report delineates situations that warrant precautions or contraindications to using a vaccine. These recommendations are intended for use in the United States because vaccine availability and use, as well as epidemiologic circumstances, differ in other countries. Individual circumstances might warrant deviations from these recommendations. The relative balance of benefits and risks can change as diseases are controlled or eradicated. For example, because wild poliovirus transmission has been interrupted in the United States since 1979, the only indigenous cases of paralytic poliomyelitis reported since that time have been caused by live oral poliovirus vaccine (OPV). In 1997, to reduce the risk for vaccine-associated paralytic polio (VAPP), increased use of inactivated poliovirus vaccine (IPV) was recommended in the United States (3). In 1999, to eliminate the risk for VAPP, exclusive use of IPV was recommended for routine vaccination in the United States (4), and OPV subsequently became unavailable for routine use. However, because of superior ability to induce intestinal immunity and to prevent spread among close contacts, OPV remains the vaccine of choice for areas where wild poliovirus is still present. Until worldwide eradication of poliovirus is accomplished, continued vaccination of the U.S. population against poliovirus will be necessary.
Timing and Spacing of Immunobiologics
General Principles for Vaccine Scheduling
Optimal response to a vaccine depends on multiple factors, including the nature of the vaccine and the age and immune status of the recipient. Recommendations for the age at which vaccines are administered are influenced by age-specific risks for disease, age-specific risks for complications, ability of persons of a certain age to respond to the vaccine, and potential interference with the immune response by passively transferred maternal antibody. Vaccines are recommended for members of the youngest age group at risk for experiencing the disease for whom efficacy and safety have been demonstrated.
Certain products, including inactivated vaccines, toxoids, recombinant subunit and polysaccharide conjugate vaccines, require administering >2 doses for development of an adequate and persisting antibody response. Tetanus and diphtheria toxoids require periodic reinforcement or booster doses to maintain protective antibody concentrations. Unconjugated polysaccharide vaccines do not induce T-cell memory, and booster doses are not expected to produce substantially increased protection. Conjugation with a protein carrier improves the effectiveness of polysaccharide vaccines by inducing T-cell--dependent immunologic function. Vaccines that stimulate both cell-mediated immunity and neutralizing antibodies (e.g., live attenuated virus vaccines) usually can induce prolonged, often lifelong immunity, even if antibody titers decline as time progresses (5). Subsequent exposure to infection usually does not lead to viremia but to a rapid anamnestic antibody response.
Approximately 90%--95% of recipients of a single dose of a parenterally administered live vaccine at the recommended age (i.e., measles, mumps, rubella [MMR], varicella, and yellow fever), develop protective antibody within 2 weeks of the dose. However, because a limited proportion of recipients (<5%) of MMR vaccine fail to respond to one dose, a second dose is recommended to provide another opportunity to develop immunity (6). The majority of persons who fail to respond to the first dose of MMR respond to a second dose (7). Similarly, approximately 20% of persons aged >13 years fail to respond to the first dose of varicella vaccine; 99% of recipients seroconvert after two doses (8).
The recommended childhood vaccination schedule is revised annually and is published each January. Recommendations for vaccination of adolescents and adults are revised less frequently, except for influenza vaccine recommendations, which are published annually. Physicians and other health-care providers should always ensure that they are following the most up-to-date schedules, which are available from CDC's National Immunization Program website at http://www.cdc.gov/nip (accessed October 11, 2001).
Spacing of Multiple Doses of the Same Antigen
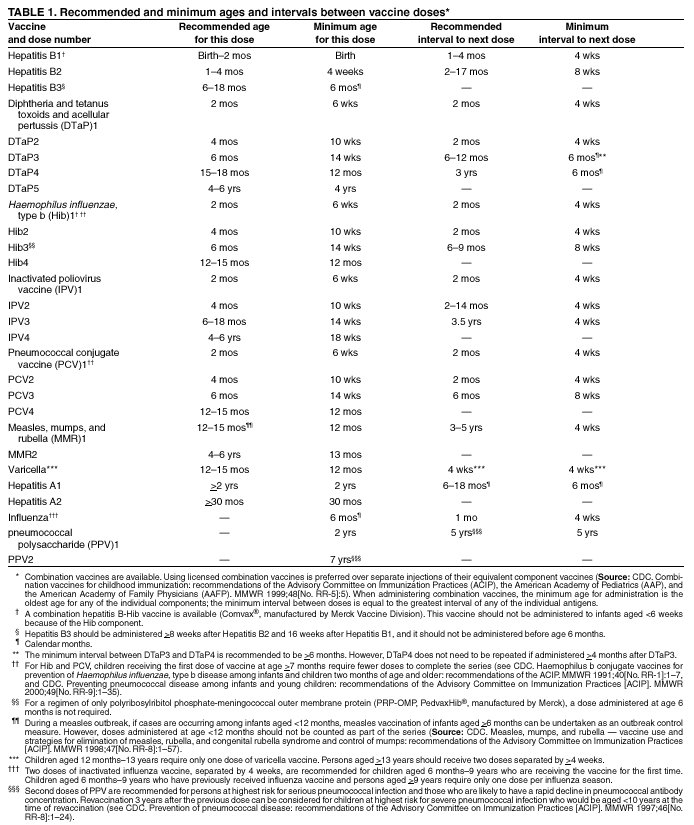
Vaccination providers are encouraged to adhere as closely as possible to the recommended childhood immunization schedule. Clinical studies have reported that recommended ages and intervals between doses of multidose antigens provide optimal protection or have the best evidence of efficacy. Recommended vaccines and recommended intervals between doses are provided in this report (Table 1).
In certain circumstances, administering doses of a multidose vaccine at shorter than the recommended intervals might be necessary. This can occur when a person is behind schedule and needs to be brought up-to-date as quickly as possible or when international travel is impending. In these situations, an accelerated schedule can be used that uses intervals between doses shorter than those recommended for routine vaccination. Although the effectiveness of all accelerated schedules has not been evaluated in clinical trials, the Advisory Committee on Immunization Practices (ACIP) believes that the immune response when accelerated intervals are used is acceptable and will lead to adequate protection. The accelerated, or minimum, intervals and ages that can be used for scheduling catch-up vaccinations is provided in this report (Table 1). Vaccine doses should not be administered at intervals less than these minimum intervals or earlier than the minimum age.*
In clinical practice, vaccine doses occasionally are administered at intervals less than the minimum interval or at ages younger than the minimum age. Doses administered too close together or at too young an age can lead to a suboptimal immune response. However, administering a dose a limited number of days earlier than the minimum interval or age is unlikely to have a substantially negative effect on the immune response to that dose. Therefore, ACIP recommends that vaccine doses administered <4 days before the minimum interval or age be counted as valid.† However, because of its unique schedule, this recommendation does not apply to rabies vaccine (9). Doses administered >5 days earlier than the minimum interval or age should not be counted as valid doses and should be repeated as age-appropriate. The repeat dose should be spaced after the invalid dose by the recommended minimum interval as provided in this report (Table 1). For example, if Haemophilus influenzae type b (Hib) doses one and two were administered only 2 weeks apart, dose two is invalid and should be repeated. The repeat dose should be administered >4 weeks after the invalid (second) dose. The repeat dose would be counted as the second valid dose. Doses administered >5 days before the minimum age should be repeated on or after the child reaches the minimum age and >4 weeks after the invalid dose. For example, if varicella vaccine were administered at age 10 months, the repeat dose would be administered no earlier than the child's first birthday.
Certain vaccines produce increased rates of local or systemic reactions in certain recipients when administered too frequently (e.g., adult tetanus-diphtheria toxoid [Td], pediatric diphtheria-tetanus toxoid [DT], and tetanus toxoid) (10,11). Such reactions are thought to result from the formation of antigen-antibody complexes. Optimal record keeping, maintaining patient histories, and adhering to recommended schedules can decrease the incidence of such reactions without adversely affecting immunity.
Simultaneous Administration
Experimental evidence and extensive clinical experience have strengthened the scientific basis for administering vaccines simultaneously (i.e., during the same office visit, not combined in the same syringe). Simultaneously administering all vaccines for which a person is eligible is critical, including for childhood vaccination programs, because simultaneous administration increases the probability that a child will be fully immunized at the appropriate age. A study conducted during a measles outbreak demonstrated that approximately one third of measles cases among unvaccinated but vaccine-eligible preschool children could have been prevented if MMR had been administered at the same visit when another vaccine was administered (12). Simultaneous administration also is critical when preparing for foreign travel and if uncertainty exists that a person will return for further doses of vaccine.
Simultaneously administering the most widely used live and inactivated vaccines have produced seroconversion rates and rates of adverse reactions similar to those observed when the vaccines are administered separately (13--16). Routinely administering all vaccines simultaneously is recommended for children who are the appropriate age to receive them and for whom no specific contraindications exist at the time of the visit. Administering combined MMR vaccine yields results similar to administering individual measles, mumps, and rubella vaccines at different sites. Therefore, no medical basis exists for administering these vaccines separately for routine vaccination instead of the preferred MMR combined vaccine (6). Administering separate antigens would result in a delay in protection for the deferred components. Response to MMR and varicella vaccines administered on the same day is identical to vaccines administered a month apart (17). No evidence exists that OPV interferes with parenterally administered live vaccines. OPV can be administered simultaneously or at any interval before or after parenteral live vaccines. No data exist regarding the immunogenicity of oral Ty21a typhoid vaccine when administered concurrently or within 30 days of live virus vaccines. In the absence of such data, if typhoid vaccination is warranted, it should not be delayed because of administration of virus vaccines (18).
Simultaneously administering pneumococcal polysaccharide vaccine and inactivated influenza vaccine elicits a satisfactory antibody response without increasing the incidence or severity of adverse reactions (19). Simultaneously administering pneumococcal polysaccharide vaccine and inactivated influenza vaccine is strongly recommended for all persons for whom both vaccines are indicated.
Hepatitis B vaccine administered with yellow fever vaccine is as safe and immunogenic as when these vaccines are administered separately (20). Measles and yellow fever vaccines have been administered safely at the same visit and without reduction of immunogenicity of each of the components (21,22).
Depending on vaccines administered in the first year of life, children aged 12--15 months can receive <7 injections during a single visit (MMR, varicella, Hib, pneumococcal conjugate, diphtheria and tetanus toxoids and acellular pertussis [DTaP], IPV, and hepatitis B vaccines). To help reduce the number of injections at the 12--15-month visit, the IPV primary series can be completed before the child's first birthday. MMR and varicella vaccines should be administered at the same visit that occurs as soon as possible on or after the first birthday. The majority of children aged 1 year who have received two (polyribosylribitol phosphate-meningococcal outer membrane protein [PRP-OMP]) or three (PRP-tetanus [PRP-T], diphtheria CRM197 [CRM, cross-reactive material] protein conjugate [HbOC]) prior doses of Hib vaccine, and three prior doses of DTaP and pneumococcal conjugate vaccine have developed protection (23,24). The third (PRP-OMP) or fourth (PRP-T, HbOC) dose of the Hib series, and the fourth doses of DTaP and pneumococcal conjugate vaccines are critical in boosting antibody titer and ensuring continued protection (24--26). However, the booster dose of the Hib or pneumococcal conjugate series can be deferred until ages 15--18 months for children who are likely to return for future visits. The fourth dose of DTaP is recommended to be administered at ages 15--18 months, but can be administered as early as age 12 months under certain circumstances (25). For infants at low risk for infection with hepatitis B virus (i.e., the mother tested negative for hepatitis B surface antigen [HBsAg] at the time of delivery and the child is not of Asian or Pacific Islander descent), the hepatitis B vaccine series can be completed at any time during ages 6--18 months. Recommended spacing of doses should be maintained (Table 1).
Use of combination vaccines can reduce the number of injections required at an office visit. Licensed combination vaccines can be used whenever any components of the combination are indicated and its other components are not contraindicated. Use of licensed combination vaccines is preferred over separate injection of their equivalent component vaccines (27). Only combination vaccines approved by the Food and Drug Administration (FDA) should be used. Individual vaccines must never be mixed in the same syringe unless they are specifically approved for mixing by FDA. Only one vaccine (DTaP and PRP-T Hib vaccine, marketed as TriHIBit® [manufactured by Aventis Pasteur]) is FDA-approved for mixing in the same syringe. This vaccine should not be used for primary vaccination in infants aged 2, 4, and 6 months, but it can be used as a booster after any Hib vaccine.
Nonsimultaneous Administration
Inactivated vaccines do not interfere with the immune response to other inactivated vaccines or to live vaccines. An inactivated vaccine can be administered either simultaneously or at any time before or after a different inactivated vaccine or live vaccine (Table 2).
The immune response to one live-virus vaccine might be impaired if administered within 30 days of another live-virus vaccine (28,29). Data are limited concerning interference between live vaccines. In a study conducted in two U.S. health maintenance organizations, persons who received varicella vaccine <30 days after MMR vaccination had an increased risk for varicella vaccine failure (i.e., varicella disease in a vaccinated person) of 2.5-fold compared with those who received varicella vaccine before or >30 days after MMR (30). In contrast, a 1999 study determined that the response to yellow fever vaccine is not affected by monovalent measles vaccine administered 1--27 days earlier (21). The effect of nonsimultaneously administering rubella, mumps, varicella, and yellow fever vaccines is unknown.
To minimize the potential risk for interference, parenterally administered live vaccines not administered on the same day should be administered >4 weeks apart whenever possible (Table 2). If parenterally administered live vaccines are separated by <4 weeks, the vaccine administered second should not be counted as a valid dose and should be repeated. The repeat dose should be administered >4 weeks after the last, invalid dose. Yellow fever vaccine can be administered at any time after single-antigen measles vaccine. Ty21a typhoid vaccine and parenteral live vaccines (i.e., MMR, varicella, yellow fever) can be administered simultaneously or at any interval before or after each other, if indicated.
Spacing of Antibody-Containing Products and Vaccines
Live Vaccines
Ty21a typhoid and yellow fever vaccines can be administered at any time before, concurrent with, or after administering any immune globulin or hyperimmune globulin (e.g., hepatitis B immune globulin and rabies immune globulin). Blood (e.g., whole blood, packed red blood cells, and plasma) and other antibody-containing blood products (e.g., immune globulin, hyperimmune globulin, and intravenous immune globulin [IGIV]) can inhibit the immune response to measles and rubella vaccines for >3 months (31,32). The effect of blood and immune globulin preparations on the response to mumps and varicella vaccines is unknown, but commercial immune globulin preparations contain antibodies to these viruses. Blood products available in the United States are unlikely to contain a substantial amount of antibody to yellow fever vaccine virus. The length of time that interference with parenteral live vaccination (except yellow fever vaccine) can persist after the antibody-containing product is a function of the amount of antigen-specific antibody contained in the product (31--33). Therefore, after an antibody-containing product is received, parenteral live vaccines (except yellow fever vaccine) should be delayed until the passive antibody has degraded (Table 3). Recommended intervals between receipt of various blood products and measles-containing vaccine and varicella vaccine are listed in this report (Table 4). If a dose of parenteral live-virus vaccine (except yellow fever vaccine) is administered after an antibody-containing product but at an interval shorter than recommended in this report, the vaccine dose should be repeated unless serologic testing indicates a response to the vaccine. The repeat dose or serologic testing should be performed after the interval indicated for the antibody-containing product (Table 4).
Although passively acquired antibodies can interfere with the response to rubella vaccine, the low dose of anti-Rho(D) globulin administered to postpartum women has not been demonstrated to reduce the response to the RA27/3 strain rubella vaccine (34). Because of the importance of rubella immunity among childbearing-age women (6,35), the postpartum vaccination of rubella-susceptible women with rubella or MMR vaccine should not be delayed because of receipt of anti-Rho(D) globulin or any other blood product during the last trimester of pregnancy or at delivery. These women should be vaccinated immediately after delivery and, if possible, tested >3 months later to ensure immunity to rubella and, if necessary, to measles (6).
Interference can occur if administering an antibody-containing product becomes necessary after administering MMR, its individual components, or varicella vaccine. Usually, vaccine virus replication and stimulation of immunity will occur 1--2 weeks after vaccination. Thus, if the interval between administering any of these vaccines and subsequent administration of an antibody-containing product is <14 days, vaccination should be repeated after the recommended interval (Tables 3,4), unless serologic testing indicates that antibodies were produced.
A humanized mouse monoclonal antibody product (palivizumab) is available for prevention of respiratory syncytial virus infection among infants and young children. This product contains only antibody to respiratory syncytial virus; hence, it will not interfere with immune response to live or inactivated vaccines.
Inactivated Vaccines
Antibody-containing products interact less with inactivated vaccines, toxoids, recombinant subunit, and polysaccharide vaccines than with live vaccines (36). Therefore, administering inactivated vaccines and toxoids either simultaneously with or at any interval before or after receipt of an antibody-containing product should not substantially impair development of a protective antibody response (Table 3). The vaccine or toxoid and antibody preparation should be administered at different sites by using the standard recommended dose. Increasing the vaccine dose volume or number of vaccinations is not indicated or recommended.
Interchangeability of Vaccines from Different Manufacturers
Numerous vaccines are available from different ma00048610.htmnufacturers, and these vaccines usually are not identical in antigen content or amount or method of formulation. Manufacturers use different production processes, and their products might contain different concentrations of antigen per dose or different stabilizers or preservatives.
Available data indicate that infants who receive sequential doses of different Hib conjugate, hepatitis B, and hepatitis A vaccines produce a satisfactory antibody response after a complete primary series (37--40). All brands of Hib conjugate, hepatitis B,§ and hepatitis A vaccines are interchangeable within their respective series. If different brands of Hib conjugate vaccine are administered, a total of three doses is considered adequate for the primary series among infants. After completing the primary series, any Hib conjugate vaccine can be used for the booster dose at ages 12--18 months.
Data are limited regarding the safety, immunogenicity, and efficacy of using acellular pertussis (as DTaP) vaccines from different manufacturers for successive doses of the pertussis series. Available data from one study indicate that, for the first three doses of the DTaP series, one or two doses of Tripedia® (manufactured by Aventis Pasteur) followed by Infanrix® (manufactured by GlaxoSmithKline) for the remaining doses(s) is comparable to three doses of Tripedia with regard to immunogenicity, as measured by antibodies to diphtheria, tetanus, and pertussis toxoid, and filamentous hemagglutinin (41). However, in the absence of a clear serologic correlate of protection for pertussis, the relevance of these immunogenicity data for protection against pertussis is unknown. Whenever feasible, the same brand of DTaP vaccine should be used for all doses of the vaccination series; however, vaccination providers might not know or have available the type of DTaP vaccine previously administered to a child. In this situation, any DTaP vaccine should be used to continue or complete the series. Vaccination should not be deferred because the brand used for previous doses is not available or is unknown (25,42).
Lapsed Vaccination Schedule
Vaccination providers are encouraged to administer vaccines as close to the recommended intervals as possible. However, longer-than-recommended intervals between doses do not reduce final antibody concentrations, although protection might not be attained until the recommended number of doses has been administered. An interruption in the vaccination schedule does not require restarting the entire series of a vaccine or toxoid or the addition of extra doses.
Unknown or Uncertain Vaccination Status
Vaccination providers frequently encounter persons who do not have adequate documentation of vaccinations. Providers should only accept written, dated records as evidence of vaccination. With the exception of pneumococcal polysaccharide vaccine (43), self-reported doses of vaccine without written documentation should not be accepted. Although vaccinations should not be postponed if records cannot be found, an attempt to locate missing records should be made by contacting previous health-care providers and searching for a personally held record. If records cannot be located, these persons should be considered susceptible and should be started on the age-appropriate vaccination schedule. Serologic testing for immunity is an alternative to vaccination for certain antigens (e.g., measles, mumps, rubella, varicella, tetanus, diphtheria, hepatitis A, hepatitis B, and poliovirus) (see Vaccination of Internationally Adopted Children).
Contraindications and Precautions
Contraindications and precautions to vaccination dictate circumstances when vaccines will not be administered. The majority of contraindications and precautions are temporary, and the vaccination can be administered later. A contraindication is a condition in a recipient that increases the risk for a serious adverse reaction. A vaccine will not be administered when a contraindication is present. For example, administering influenza vaccine to a person with an anaphylactic allergy to egg protein could cause serious illness in or death of the recipient.
National standards for pediatric immunization practices have been established and include true contraindications and precautions to vaccination (Table 5) (1). The only true contraindication applicable to all vaccines is a history of a severe allergic reaction after a prior dose of vaccine or to a vaccine constituent (unless the recipient has been desensitized). Severely immunocompromised persons should not receive live vaccines. Children who experience an encephalopathy <7 days after administration of a previous dose of diphtheria and tetanus toxoids and whole-cell pertussis vaccine (DTP) or DTaP not attributable to another identifiable cause should not receive further doses of a vaccine that contains pertussis. Because of the theoretical risk to the fetus, women known to be pregnant should not receive live attenuated virus vaccines (see Vaccination During Pregnancy).
A precaution is a condition in a recipient that might increase the risk for a serious adverse reaction or that might compromise the ability of the vaccine to produce immunity (e.g., administering measles vaccine to a person with passive immunity to measles from a blood transfusion). Injury could result, or a person might experience a more severe reaction to the vaccine than would have otherwise been expected; however, the risk for this happening is less than expected with a contraindication. Under normal circumstances, vaccinations should be deferred when a precaution is present. However, a vaccination might be indicated in the presence of a precaution because the benefit of protection from the vaccine outweighs the risk for an adverse reaction. For example, caution should be exercised in vaccinating a child with DTaP who, within 48 hours of receipt of a prior dose of DTP or DTaP, experienced fever >40.5C (105F); had persistent, inconsolable crying for >3 hours; collapsed or experienced a shock-like state; or had a seizure <3 days after receiving the previous dose of DTP or DTaP. However, administering a pertussis-containing vaccine should be considered if the risk for pertussis is increased (e.g., during a pertussis outbreak) (25). The presence of a moderate or severe acute illness with or without a fever is a precaution to administration of all vaccines. Other precautions are listed in this report (Table 5).
Physicians and other health-care providers might inappropriately consider certain conditions or circumstances to be true contraindications or precautions to vaccination. This misconception results in missed opportunities to administer recommended vaccines (44). Likewise, physicians and other health-care providers might fail to understand what constitutes a true contraindication or precaution and might administer a vaccine when it should be withheld. This practice can result in an increased risk for an adverse reaction to the vaccine. Conditions often inappropriately regarded as contraindications to vaccination are listed in this report (Table 5). Among the most common are diarrhea and minor upper-respiratory tract illnesses (including otitis media) with or without fever, mild to moderate local reactions to a previous dose of vaccine, current antimicrobial therapy, and the convalescent phase of an acute illness.
The decision to administer or delay vaccination because of a current or recent acute illness depends on the severity of symptoms and the etiology of the disease. All vaccines can be administered to persons with minor acute illness (e.g., diarrhea or mild upper-respiratory tract infection with or without fever). Studies indicate that failure to vaccinate children with minor illnesses can seriously impede vaccination efforts (45--47). Among persons whose compliance with medical care cannot be ensured, use of every opportunity to provide appropriate vaccinations is critical.
The majority of studies support the safety and efficacy of vaccinating persons who have mild illness (48--50). For example, in the United States, >97% of children with mild illnesses produced measles antibody after vaccination (51). Only one limited study has reported a lower rate of seroconversion (79%) to the measles component of MMR vaccine among children with minor, afebrile upper-respiratory tract infections (52). Therefore, vaccination should not be delayed because of the presence of mild respiratory tract illness or other acute illness with or without fever.
Persons with moderate or severe acute illness should be vaccinated as soon as they have recovered from the acute phase of the illness. This precaution avoids superimposing adverse effects of the vaccine on the underlying illness or mistakenly attributing a manifestation of the underlying illness to the vaccine.
Routine physical examinations and measuring temperatures are not prerequisites for vaccinating infants and children who appear to be healthy. Asking the parent or guardian if the child is ill and then postponing vaccination for those with moderate to severe illness, or proceeding with vaccination if no contraindications exist, are appropriate procedures in childhood immunization programs.
A family history of seizures or other central nervous system disorders is not a contraindication to administration of pertussis or other vaccines. However, delaying pertussis vaccination for infants and children with a history of previous seizures until the child's neurologic status has been assessed is prudent. Pertussis vaccine should not be administered to infants with evolving neurologic conditions until a treatment regimen has been established and the condition has stabilized (25).
Vaccine Administration
Infection Control and Sterile Technique
Persons administering vaccines should follow necessary precautions to minimize risk for spreading disease. Hands should be washed with soap and water or cleansed with an alcohol-based waterless antiseptic hand rub between each patient contact. Gloves are not required when administering vaccinations, unless persons administering vaccinations are likely to come into contact with potentially infectious body fluids or have open lesions on their hands. Syringes and needles used for injections must be sterile and disposable to minimize the risk of contamination. A separate needle and syringe should be used for each injection. Changing needles between drawing vaccine from a vial and injecting it into a recipient is unnecessary. Different vaccines should never be mixed in the same syringe unless specifically licensed for such use.
Disposable needles and syringes should be discarded in labeled, puncture-proof containers to prevent inadvertent needle-stick injury or reuse. Safety needles or needle-free injection devices also can reduce the risk for injury and should be used whenever available (see Occupational Safety Regulations).
Recommended Routes of Injection and Needle Length
Routes of administration are recommended by the manufacturer for each immunobiologic. Deviation from the recommended route of administration might reduce vaccine efficacy (53,54) or increase local adverse reactions (55--57). Injectable immunobiologics should be administered where the likelihood of local, neural, vascular, or tissue injury is limited. Vaccines containing adjuvants should be injected into the muscle mass; when administered subcutaneously or intradermally, they can cause local irritation, induration, skin discoloration, inflammation, and granuloma formation.
Subcutaneous Injections
Subcutaneous injections usually are administered at a 45-degree angle into the thigh of infants aged <12 months and in the upper-outer triceps area of persons aged >12 months. Subcutaneous injections can be administered into the upper-outer triceps area of an infant, if necessary. A 5/8-inch, 23--25-gauge needle should be inserted into the subcutaneous tissue.
Intramuscular Injections
Intramuscular injections are administered at a 90-degree angle into the anterolateral aspect of the thigh or the deltoid muscle of the upper arm. The buttock should not be used for administration of vaccines or toxoids because of the potential risk of injury to the sciatic nerve (58). In addition, injection into the buttock has been associated with decreased immunogenicity of hepatitis B and rabies vaccines in adults, presumably because of inadvertent subcutaneous injection or injection into deep fat tissue (53,59).
For all intramuscular injections, the needle should be long enough to reach the muscle mass and prevent vaccine from seeping into subcutaneous tissue, but not so long as to involve underlying nerves and blood vessels or bone (54,60--62). Vaccinators should be familiar with the anatomy of the area into which they are injecting vaccine. An individual decision on needle size and site of injection must be made for each person on the basis of age, the volume of the material to be administered, the size of the muscle, and the depth below the muscle surface into which the material is to be injected.
Although certain vaccination specialists advocate aspiration (i.e., the syringe plunger pulled back before injection), no data exist to document the necessity for this procedure. If aspiration results in blood in the needle hub, the needle should be withdrawn and a new site should be selected.
Infants (persons aged <12 months). Among the majority of infants, the anterolateral aspect of the thigh provides the largest muscle mass and is therefore the recommended site for injection. For the majority of infants, a 7/8--1-inch, 22--25-gauge needle is sufficient to penetrate muscle in the infant's thigh.
Toddlers and Older Children (persons aged >12 months--18 years). The deltoid muscle can be used if the muscle mass is adequate. The needle size can range from 22 to 25 gauge and from 7/8 to 1¼ inches, on the basis of the size of the muscle. For toddlers, the anterolateral thigh can be used, but the needle should be longer, usually 1 inch.
Adults (persons aged >18 years). For adults, the deltoid muscle is recommended for routine intramuscular vaccinations. The anterolateral thigh can be used. The suggested needle size is 1--1½ inches and 22--25 gauge.
Intradermal Injections
Intradermal injections are usually administered on the volar surface of the forearm. With the bevel facing upwards, a 3/8--3/4-inch, 25--27-gauge needle can be inserted into the epidermis at an angle parallel to the long axis of the forearm. The needle should be inserted so that the entire bevel penetrates the skin and the injected solution raises a small bleb. Because of the small amounts of antigen used in intradermal vaccinations, care must be taken not to inject the vaccine subcutaneously because it can result in a suboptimal immunologic response.
Multiple Vaccinations
If >2 vaccine preparations are administered or if vaccine and an immune globulin preparation are administered simultaneously, each preparation should be administered at a different anatomic site. If >2 injections must be administered in a single limb, the thigh is usually the preferred site because of the greater muscle mass; the injections should be sufficiently separated (i.e., >1 inch) so that any local reactions can be differentiated (55,63). For older children and adults, the deltoid muscle can be used for multiple intramuscular injections, if necessary. The location of each injection should documented in the person's medical record.
Jet Injection
Jet injectors (JIs) are needle-free devices that drive liquid medication through a nozzle orifice, creating a narrow stream under high pressure that penetrates skin to deliver a drug or vaccine into intradermal, subcutaneous, or intramuscular tissues (64,65). Increasing attention to JI technology as an alternative to conventional needle injection has resulted from recent efforts to reduce the frequency of needle-stick injuries to health-care workers (66) and to overcome the improper reuse and other drawbacks of needles and syringes in economically developing countries (67--69). JIs have been reported safe and effective in administering different live and inactivated vaccines for viral and bacterial diseases (69). The immune responses generated are usually equivalent to, and occasionally greater than, those induced by needle injection. However, local reactions or injury (e.g., redness, induration, pain, blood, and ecchymosis at the injection site) can be more frequent for vaccines delivered by JIs compared with needle injection (65,69).
Certain JIs were developed for situations in which substantial numbers of persons must be vaccinated rapidly, but personnel or supplies are insufficient to do so with conventional needle injection. Such high-workload devices vaccinate consecutive patients from the same nozzle orifice, fluid pathway, and dose chamber, which is refilled automatically from attached vials containing <50 doses each. Since the 1950s, these devices have been used extensively among military recruits and for mass vaccination campaigns for disease control and eradication (64). An outbreak of hepatitis B among patients receiving injections from a multiple-use--nozzle JI was documented (70,71), and subsequent laboratory, field, and animal studies demonstrated that such devices could become contaminated with blood (69,72,73).
No U.S.-licensed, high-workload vaccination devices of unquestioned safety are available to vaccination programs. Efforts are under way for the research and development of new high-workload JIs using disposable-cartridge technology that avoids reuse of any unsterilized components having contact with the medication fluid pathway or patient's blood. Until such devices become licensed and available, the use of existing multiple-use--nozzle JIs should be limited. Use can be considered when the theoretical risk for bloodborne disease transmission is outweighed by the benefits of rapid vaccination with limited personnel in responding to serious disease threats (e.g., pandemic influenza or bioterrorism event), and by any competing risks of iatrogenic or occupational infections resulting from conventional needles and syringes. Before such emergency use of multiple-use--nozzle JIs, health-care workers should consult with local, state, national, or international health agencies or organizations that have experience in their use.
In the 1990s, a new generation of low-workload JIs were introduced with disposable cartridges serving as dose chambers and nozzle (69). With the provision of a new sterile cartridge for each patient and other correct use, these devices avoid the safety concerns described previously for multiple-use--nozzle devices. They can be used in accordance with their labeling for intradermal, subcutaneous, or intramuscular administration.
Methods for Alleviating Discomfort and Pain Associated with Vaccination
Comfort measures and distraction techniques (e.g., playing music or pretending to blow away the pain) might help children cope with the discomfort associated with vaccination. Pretreatment (30-60 minutes before injection) with 5% topical lidocaine-prilocaine emulsion (EMLA® cream or disk [manufactured by AstraZeneca LP]) can decrease the pain of vaccination among infants by causing superficial anesthesia (74,75). Preliminary evidence indicates that this cream does not interfere with the immune response to MMR (76). Topical lidocaine-prilocaine emulsion should not be used on infants aged <12 months who are receiving treatment with methemoglobin-inducing agents because of the possible development of methemoglobinemia (77). Acetaminophen has been used among children to reduce the discomfort and fever associated with vaccination (78). However, acetaminophen can cause formation of methemoglobin and, thus, might interact with lidocaine-prilocaine cream, if used concurrently (77). Ibuprofen or other nonaspirin analgesic can be used, if necessary. Use of a topical refrigerant (vapocoolant) spray can reduce the short-term pain associated with injections and can be as effective as lidocaine-prilocaine cream (79). Administering sweet-tasting fluid orally immediately before injection can result in a calming or analgesic effect among certain infants.
Nonstandard Vaccination Practices
Recommendations regarding route, site, and dosage of immunobiologics are derived from data from clinical trials, from practical experience, and from theoretical considerations. ACIP strongly discourages variations from the recommended route, site, volume, or number of doses of any vaccine.
Variation from the recommended route and site can result in inadequate protection. The immunogenicity of hepatitis B vaccine and rabies vaccine is substantially lower when the gluteal rather than the deltoid site is used for administration (53,59). Hepatitis B vaccine administered intradermally can result in a lower seroconversion rate and final titer of hepatitis B surface antibody than when administered by the deltoid intramuscular route (80,81). Doses of rabies vaccine administered in the gluteal site should not be counted as valid doses and should be repeated. Hepatitis B vaccine administered by any route or site other than intramuscularly in the anterolateral thigh or deltoid muscle should not be counted as valid and should be repeated, unless serologic testing indicates that an adequate response has been achieved.
Live attenuated parenteral vaccines (e.g., MMR, varicella, or yellow fever) and certain inactivated vaccines (e.g., IPV, pneumococcal polysaccharide, and anthrax) are recommended by the manufacturers to be administered by subcutaneous injection. Pneumococcal polysaccharide and IPV are approved for either intramuscular or subcutaneous administration. Response to these vaccines probably will not be affected if the vaccines are administered by the intramuscular rather then subcutaneous route. Repeating doses of vaccine administered by the intramuscular route rather than by the subcutaneous route is unnecessary.
Administering volumes smaller than those recommended (e.g., split doses) can result in inadequate protection. Using larger than the recommended dose can be hazardous because of excessive local or systemic concentrations of antigens or other vaccine constituents. Using multiple reduced doses that together equal a full immunizing dose or using smaller divided doses is not endorsed or recommended. Any vaccination using less than the standard dose should not be counted, and the person should be revaccinated according to age, unless serologic testing indicates that an adequate response has been achieved.
Preventing Adverse Reactions
Vaccines are intended to produce active immunity to specific antigens. An adverse reaction is an untoward effect that occurs after a vaccination that is extraneous to the vaccine's primary purpose of producing immunity. Adverse reactions also are called vaccine side effects.
All vaccines might cause adverse reactions (82). Vaccine adverse reactions are classified by three general categories: local, systemic, and allergic. Local reactions are usually the least severe and most frequent. Systemic reactions (e.g., fever) occur less frequently than local reactions. Serious allergic reactions (e.g., anaphylaxis) are the most severe and least frequent. Severe adverse reactions are rare.
The key to preventing the majority of serious adverse reactions is screening. Every person who administers vaccines should screen patients for contraindications and precautions to the vaccine before it is administered (Table 5). Standardized screening questionnaires have been developed and are available from certain state immunization programs and other sources (e.g., the Immunization Action Coalition at http://www.immunize.org [accessed October 31, 2001]).
Severe allergic reactions after vaccination are rare. However, all physicians and other health-care providers who administer vaccines should have procedures in place for the emergency management of a person who experiences an anaphylactic reaction. All vaccine providers should be familiar with the office emergency plan and be certified in cardiopulmonary resuscitation.
Syncope (vasovagal or vasodepressor reaction) can occur after vaccination, most commonly among adolescents and young adults. During 1990--August 2001, a total of 2,269 reports to the Vaccine Adverse Event Reporting system were coded as syncope. Forty percent of these episodes were reported among persons aged 10--18 years (CDC, unpublished data, 2001). Approximately 12% of reported syncopal episodes resulted in hospitalization because of injury or medical evaluation. Serious injury, including skull fractures and cerebral bleeding, have been reported to result from syncopal episodes after vaccination. A published review of syncope after vaccination reported that 63% of syncopal episodes occurred <5 minutes after vaccination, and 89% occurred within 15 minutes after vaccination (83). Although syncopal episodes are uncommon and serious allergic reactions are rare, certain vaccination specialists recommend that persons be observed for 15--20 minutes after being vaccinated, if possible (84). If syncope develops, patients should be observed until the symptoms resolve.
Managing Acute Vaccine Reactions
Although rare after vaccination, the immediate onset and life-threatening nature of an anaphylactic reaction require that personnel and facilities providing vaccinations be capable of providing initial care for suspected anaphylaxis. Epinephrine and equipment for maintaining an airway should be available for immediate use.
Anaphylaxis usually begins within minutes of vaccine administration. Rapidly recognizing and initiating treatment are required to prevent possible progression to cardiovascular collapse. If flushing, facial edema, urticaria, itching, swelling of the mouth or throat, wheezing, difficulty breathing, or other signs of anaphylaxis occur, the patient should be placed in a recumbent position with the legs elevated. Aqueous epinephrine (1:1000) should be administered and can be repeated within 10--20 minutes (84). A dose of diphenhydramine hydrochloride might shorten the reaction, but it will have little immediate effect. Maintenance of an airway and oxygen administration might be necessary. Arrangements should be made for immediate transfer to an emergency facility for further evaluation and treatment.
Occupational Safety Regulations
Bloodborne diseases (e.g., hepatitis B and C and human immunodeficiency virus [HIV]) are occupational hazards for health-care workers. In November 2000, to reduce the incidence of needle-stick injuries among health-care workers and the consequent risk for bloodborne diseases acquired from patients, the Needlestick Safety and Prevention Act was signed into law. The act directed the Occupational Safety and Health Administration (OSHA) to strengthen its existing bloodborne pathogen standards. Those standards were revised and became effective in April 2001 (66). These federal regulations require that safer injection devices (e.g., needle-shielding syringes or needle-free injectors) be used for parenteral vaccination in all clinical settings when such devices are appropriate, commercially available, and capable of achieving the intended clinical purpose. The rules also require that records be kept documenting the incidence of injuries caused by medical sharps (except in workplaces with <10 employees) and that nonmanagerial employees be involved in the evaluation and selection of safer devices to be procured.
Needle-shielding or needle-free devices that might satisfy the occupational safety regulations for administering parenteral injections are available in the United States and are listed at multiple websites (69,85--87).¶ Additional information regarding implementation and enforcement of these regulations is available at the OSHA website at http://www.osha-slc.gov/needlesticks (accessed October 31, 2001).
Storage and Handling of Immunobiologics
Failure to adhere to recommended specifications for storage and handling of immunobiologics can reduce potency, resulting in an inadequate immune response in the recipient. Recommendations included in a product's package insert, including reconstitution of the vaccine, should be followed carefully. Vaccine quality is the shared responsibility of all parties from the time the vaccine is manufactured until administration. All vaccines should be inspected upon delivery and monitored during storage to ensure that the cold chain has been maintained. Vaccines should continue to be stored at recommended temperatures immediately upon receipt. Certain vaccines (e.g., MMR, varicella, and yellow fever) are sensitive to increased temperature. All other vaccines are sensitive to freezing. Mishandled vaccine usually is not distinguishable from potent vaccine. When in doubt regarding the appropriate handling of a vaccine, vaccination providers should contact the manufacturer. Vaccines that have been mishandled (e.g., inactivated vaccines and toxoids that have been exposed to freezing temperatures) or that are beyond their expiration date should not be administered. If mishandled or expired vaccines are administered inadvertently, they should not be counted as valid doses and should be repeated, unless serologic testing indicates a response to the vaccine.
Live attenuated virus vaccines should be administered promptly after reconstitution. Varicella vaccine must be administered <30 minutes after reconstitution. Yellow fever vaccine must be used <1 hour after reconstitution. MMR vaccine must be administered <8 hours after reconstitution. If not administered within these prescribed time periods after reconstitution, the vaccine must be discarded.
The majority of vaccines have a similar appearance after being drawn into a syringe. Instances in which the wrong vaccine inadvertently was administered are attributable to the practice of prefilling syringes or drawing doses of a vaccine into multiple syringes before their immediate need. ACIP discourages the routine practice of prefilling syringes because of the potential for such administration errors. To prevent errors, vaccine doses should not be drawn into a syringe until immediately before administration. In certain circumstances where a single vaccine type is being used (e.g., in advance of a community influenza vaccination campaign), filling multiple syringes before their immediate use can be considered. Care should be taken to ensure that the cold chain is maintained until the vaccine is administered. When the syringes are filled, the type of vaccine, lot number, and date of filling must be carefully labeled on each syringe, and the doses should be administered as soon as possible after filling.
Certain vaccines are distributed in multidose vials. When opened, the remaining doses from partially used multidose vials can be administered until the expiration date printed on the vial or vaccine packaging, provided that the vial has been stored correctly and that the vaccine is not visibly contaminated.
Special Situations
Concurrently Administering Antimicrobial Agents and Vaccines
With limited exceptions, using an antibiotic is not a contraindication to vaccination. Antimicrobial agents have no effect on the response to live attenuated vaccines, except live oral Ty21a typhoid vaccine, and have no effect on inactivated, recombinant subunit, or polysaccharide vaccines or toxoids. Ty21a typhoid vaccine should not be administered to persons receiving antimicrobial agents until >24 hours after any antibiotic dose (18).
Antiviral drugs used for treatment or prophylaxis of influenza virus infections have no effect on the response to inactivated influenza vaccine (88). Antiviral drugs active against herpesviruses (e.g., acyclovir or valacyclovir) might reduce the efficacy of live attenuated varicella vaccine. These drugs should be discontinued >24 hours before administration of varicella vaccine, if possible.
The antimalarial drug mefloquine (Lariam® [manufactured by Roche Laboratories, Inc.]) could affect the immune response to oral Ty21a typhoid vaccine if both are taken simultaneously (89,90). To minimize this effect, administering Ty21a typhoid vaccine >24 hours before or after a dose of mefloquine is prudent.
Tuberculosis Screening and Skin Test Reactivity
Measles illness, severe acute or chronic infections, HIV infection, and malnutrition can create an anergic state during which the tuberculin skin test (usually known as purified protein derivative [PPD] skin test) might give a false negative reaction (91--93). Although any live attenuated measles vaccine can theoretically suppress PPD reactivity, the degree of suppression is probably less than that occurring from acute infection from wild measles virus. Although routine PPD screening of all children is no longer recommended, PPD screening is sometimes needed at the same time as administering a measles-containing vaccine (e.g., for well-child care, school entrance, or for employee health reasons), and the following options should be considered:
No data exist for the potential degree of PPD suppression that might be associated with other parenteral live attenuated virus vaccines (e.g., varicella or yellow fever). Nevertheless, in the absence of data, following guidelines for measles-containing vaccine when scheduling PPD screening and administering other parenteral live attenuated virus vaccines is prudent. If a risk exists that the opportunity to vaccinate might be missed, vaccination should not be delayed only because of these theoretical considerations.
Mucosally administered live attenuated virus vaccines (e.g., OPV and intranasally administered influenza vaccine) are unlikely to affect the response to PPD. No evidence has been reported that inactivated vaccines, polysaccharide vaccines, recombinant, or subunit vaccines, or toxoids interfere with response to PPD.
PPD reactivity in the absence of tuberculosis disease is not a contraindication to administration of any vaccine, including parenteral live attenuated virus vaccines. Tuberculosis disease is not a contraindication to vaccination, unless the person is moderately or severely ill. Although no studies have reported the effect of MMR vaccine on persons with untreated tuberculosis, a theoretical basis exists for concern that measles vaccine might exacerbate tuberculosis (6). Consequently, before administering MMR to persons with untreated active tuberculosis, initiating antituberculosis therapy is advisable (6). Ruling out concurrent immunosuppression (e.g., immunosuppression caused by HIV infection) before administering live attenuated vaccines is also prudent.
Severe Allergy to Vaccine Components
Vaccine components can cause allergic reactions among certain recipients. These reactions can be local or systemic and can include mild to severe anaphylaxis or anaphylactic-like responses (e.g., generalized urticaria or hives, wheezing, swelling of the mouth and throat, difficulty breathing, hypotension, and shock). Allergic reactions might be caused by the vaccine antigen, residual animal protein, antimicrobial agents, preservatives, stabilizers, or other vaccine components (94). An extensive listing of vaccine components, their use, and the vaccines that contain each component has been published (95) and is also available from CDC's National Immunization Program website at http://www.cdc.gov/nip (accessed October 31, 2001).
The most common animal protein allergen is egg protein, which is found in vaccines prepared by using embryonated chicken eggs (influenza and yellow fever vaccines). Ordinarily, persons who are able to eat eggs or egg products safely can receive these vaccines; persons with histories of anaphylactic or anaphylactic-like allergy to eggs or egg proteins should not be administered these vaccines. Asking persons if they can eat eggs without adverse effects is a reasonable way to determine who might be at risk for allergic reactions from receiving yellow fever and influenza vaccines. A regimen for administering influenza vaccine to children with egg hypersensitivity and severe asthma has been developed (96).
Measles and mumps vaccine viruses are grown in chick embryo fibroblast tissue culture. Persons with a serious egg allergy can receive measles- or mumps-containing vaccines without skin testing or desensitization to egg protein (6). Rubella and varicella vaccines are grown in human diploid cell cultures and can safely be administered to persons with histories of severe allergy to eggs or egg proteins. The rare serious allergic reaction after measles or mumps vaccination or MMR are not believed to be caused by egg antigens, but to other components of the vaccine (e.g., gelatin) (97--100). MMR, its component vaccines, and other vaccines contain hydrolyzed gelatin as a stabilizer. Extreme caution should be exercised when administering vaccines that contain gelatin to persons who have a history of an anaphylactic reaction to gelatin or gelatin-containing products. Before administering gelatin-containing vaccines to such persons, skin testing for sensitivity to gelatin can be considered. However, no specific protocols for this approach have been published.
Certain vaccines contain trace amounts of antibiotics or other preservatives (e.g., neomycin or thimerosal) to which patients might be severely allergic. The information provided in the vaccine package insert should be reviewed carefully before deciding if the rare patient with such allergies should receive the vaccine. No licensed vaccine contains penicillin or penicillin derivatives.
Certain vaccines contain trace amounts of neomycin. Persons who have experienced anaphylactic reactions to neomycin should not receive these vaccines. Most often, neomycin allergy is a contact dermatitis, a manifestation of a delayed type (cell-mediated) immune response, rather than anaphylaxis (101,102). A history of delayed type reactions to neomycin is not a contraindication for administration of these vaccines.
Thimerosal is an organic mercurial compound in use since the 1930s and added to certain immunobiologic products as a preservative. A joint statement issued by the U.S. Public Health Service and the American Academy of Pediatrics (AAP) in 1999 (103) and agreed to by the American Academy of Family Physicians (AAFP) later in 1999, established the goal of removing thimerosal as soon as possible from vaccines routinely recommended for infants. Although no evidence exists of any harm caused by low levels of thimerosal in vaccines and the risk was only theoretical (104), this goal was established as a precautionary measure.
The public is concerned about the health effects of mercury exposure of any type, and the elimination of mercury from vaccines was judged a feasible means of reducing an infant's total exposure to mercury in a world where other environmental sources of exposure are more difficult or impossible to eliminate (e.g., certain foods). Since mid-2001, vaccines routinely recommended for children have been manufactured without thimerosal as a preservative and contain either no thimerosal or only trace amounts. Thimerosal as a preservative is present in certain other vaccines (e.g., Td, DT, one of two adult hepatitis B vaccines, and influenza vaccine). A trace thimerosal formulation of one brand of influenza vaccine was licensed by FDA in September 2001.
Receiving thimerosal-containing vaccines has been believed to lead to induction of allergy. However, limited scientific basis exists for this assertion (94). Hypersensitivity to thimerosal usually consists of local delayed type hypersensitivity reactions (105--107). Thimerosal elicits positive delayed type hypersensitivity patch tests in 1%--18% of persons tested, but these tests have limited or no clinical relevance (108,109). The majority of patients do not experience reactions to thimerosal administered as a component of vaccines even when patch or intradermal tests for thimerosal indicate hypersensitivity (109). A localized or delayed type hypersensitivity reaction to thimerosal is not a contraindication to receipt of a vaccine that contains thimerosal.
Latex Allergy
Latex is liquid sap from the commercial rubber tree. Latex contains naturally occurring impurities (e.g., plant proteins and peptides), which are believed to be responsible for allergic reactions. Latex is processed to form natural rubber latex and dry natural rubber. Dry natural rubber and natural rubber latex might contain the same plant impurities as latex but in lesser amounts. Natural rubber latex is used to produce medical gloves, catheters, and other products. Dry natural rubber is used in syringe plungers, vial stoppers, and injection ports on intravascular tubing. Synthetic rubber and synthetic latex also are used in medical gloves, syringe plungers, and vial stoppers. Synthetic rubber and synthetic latex do not contain natural rubber or natural latex, and therefore, do not contain the impurities linked to allergic reactions.
The most common type of latex sensitivity is contact-type (type 4) allergy, usually as a result of prolonged contact with latex-containing gloves (110). However, injection-procedure--associated latex allergies among patients with diabetes have been described (111--113). Allergic reactions (including anaphylaxis) after vaccination procedures are rare. Only one report of an allergic reaction after administering hepatitis B vaccine in a patient with known severe allergy (anaphylaxis) to latex has been published (114).
If a person reports a severe (anaphylactic) allergy to latex, vaccines supplied in vials or syringes that contain natural rubber should not be administered, unless the benefit of vaccination outweighs the risk of an allergic reaction to the vaccine. For latex allergies other than anaphylactic allergies (e.g., a history of contact allergy to latex gloves), vaccines supplied in vials or syringes that contain dry natural rubber or natural rubber latex can be administered.
Vaccination of Premature Infants
In the majority of cases, infants born prematurely, regardless of birth weight, should be vaccinated at the same chronological age and according to the same schedule and precautions as full-term infants and children. Birth weight and size are not factors in deciding whether to postpone routine vaccination of a clinically stable premature infant (115--117), except for hepatitis B vaccine. The full recommended dose of each vaccine should be used. Divided or reduced doses are not recommended (118).
Studies demonstrate that decreased seroconversion rates might occur among certain premature infants with low birth weights (i.e., <2,000 grams) after administration of hepatitis B vaccine at birth (119). However, by chronological age 1 month, all premature infants, regardless of initial birth weight or gestational age are as likely to respond as adequately as older and larger infants (120--122). A premature infant born to HBsAg-positive mothers and mothers with unknown HBsAg status must receive immunoprophylaxis with hepatitis B vaccine and hepatitis B immunoglobulin (HBIG) <12 hours after birth. If these infants weigh <2,000 grams at birth, the initial vaccine dose should not be counted towards completion of the hepatitis B vaccine series, and three additional doses of hepatitis B vaccine should be administered, beginning when the infant is age 1 month. The optimal timing of the first dose of hepatitis B vaccine for premature infants of HBsAg-negative mothers with a birth weight of <2,000 grams has not been determined. However, these infants can receive the first dose of the hepatitis B vaccine series at chronological age 1 month. Premature infants discharged from the hospital before chronological age 1 month can also be administered hepatitis B vaccine at discharge, if they are medically stable and have gained weight consistently.
Breast-Feeding and Vaccination
Neither inactivated nor live vaccines administered to a lactating woman affect the safety of breast-feeding for mothers or infants. Breast-feeding does not adversely affect immunization and is not a contraindication for any vaccine. Limited data indicate that breast-feeding can enhance the response to certain vaccine antigens (123). Breast-fed infants should be vaccinated according to routine recommended schedules (124--126).
Although live vaccines multiply within the mother's body, the majority have not been demonstrated to be excreted in human milk. Although rubella vaccine virus might be excreted in human milk, the virus usually does not infect the infant. If infection does occur, it is well-tolerated because the viruses are attenuated (127). Inactivated, recombinant, subunit, polysaccharide, conjugate vaccines and toxoids pose no risk for mothers who are breast-feeding or for their infants.
Vaccination During Pregnancy
Risk to a developing fetus from vaccination of the mother during pregnancy is primarily theoretical. No evidence exists of risk from vaccinating pregnant women with inactivated virus or bacterial vaccines or toxoids (128,129). Benefits of vaccinating pregnant women usually outweigh potential risks when the likelihood of disease exposure is high, when infection would pose a risk to the mother or fetus, and when the vaccine is unlikely to cause harm.
Td toxoid is indicated routinely for pregnant women. Previously vaccinated pregnant women who have not received a Td vaccination within the last 10 years should receive a booster dose. Pregnant women who are not immunized or only partially immunized against tetanus should complete the primary series (130). Depending on when a woman seeks prenatal care and the required interval between doses, one or two doses of Td can be administered before delivery. Women for whom the vaccine is indicated, but who have not completed the recommended three-dose series during pregnancy, should receive follow-up after delivery to ensure the series is completed.
Women in the second and third trimesters of pregnancy have been demonstrated to be at increased risk for hospitalization from influenza (131). Therefore, routine influenza vaccination is recommended for healthy women who will be beyond the first trimester of pregnancy (i.e., >14 weeks of gestation) during influenza season (usually December--March in the United States) (88). Women who have medical conditions that increase their risk for complications of influenza should be vaccinated before the influenza season, regardless of the stage of pregnancy.
IPV can be administered to pregnant women who are at risk for exposure to wild-type poliovirus infection (4). Hepatitis B vaccine is recommended for pregnant women at risk for hepatitis B virus infection (132). Hepatitis A, pneumococcal polysaccharide, and meningococcal polysaccharide vaccines should be considered for women at increased risk for those infections (43,133,134).
Pregnant women who must travel to areas where the risk for yellow fever is high should receive yellow fever vaccine, because the limited theoretical risk from vaccination is substantially outweighed by the risk for yellow fever infection (22,135). Pregnancy is a contraindication for measles, mumps, rubella, and varicella vaccines. Although of theoretical concern, no cases of congenital rubella or varicella syndrome or abnormalities attributable to fetal infection have been observed among infants born to susceptible women who received rubella or varicella vaccines during pregnancy (6,136). Because of the importance of protecting women of childbearing age against rubella, reasonable practices in any immunization program include asking women if they are pregnant or intend to become pregnant in the next 4 weeks, not vaccinating women who state that they are pregnant, explaining the potential risk for the fetus to women who state that they are not pregnant, and counseling women who are vaccinated not to become pregnant during the 4 weeks after MMR vaccination (6,35,137). Routine pregnancy testing of women of childbearing age before administering a live-virus vaccine is not recommended (6). If a pregnant woman is inadvertently vaccinated or if she becomes pregnant within 4 weeks after MMR or varicella vaccination, she should be counseled regarding the theoretical basis of concern for the fetus; however, MMR or varicella vaccination during pregnancy should not ordinarily be a reason to terminate pregnancy (6,8).
Persons who receive MMR vaccine do not transmit the vaccine viruses to contacts (6). Transmission of varicella vaccine virus to contacts is rare (138). MMR and varicella vaccines should be administered when indicated to the children and other household contacts of pregnant women (6,8).
All pregnant women should be evaluated for immunity to rubella and be tested for the presence of HBsAg (6,35,132). Women susceptible to rubella should be vaccinated immediately after delivery. A woman known to be HBsAg-positive should be followed carefully to ensure that the infant receives HBIG and begins the hepatitis B vaccine series <12 hours after birth and that the infant completes the recommended hepatitis B vaccine series (132). No known risk exists for the fetus from passive immunization of pregnant women with immune globulin preparations.
Vaccination of Internationally Adopted Children
The ability of a clinician to determine that a person is protected on the basis of their country of origin and their records alone is limited. Internationally adopted children should receive vaccines according to recommended schedules for children in the United States. Only written documentation should be accepted as evidence of prior vaccination. Written records are more likely to predict protection if the vaccines, dates of administration, intervals between doses, and the child's age at the time of immunization are comparable to the current U.S. recommendations. Although vaccines with inadequate potency have been produced in other countries (139,140), the majority of vaccines used worldwide are produced with adequate quality control standards and are potent.
The number of American families adopting children from outside the United States has increased substantially in recent years (141). Adopted children's birth countries often have immunization schedules that differ from the recommended childhood immunization schedule in the United States. Differences in the U.S. immunization schedule and those used in other countries include the vaccines administered, the recommended ages of administration, and the number and timing of doses.
Data are inconclusive regarding the extent to which an internationally adopted child's immunization record reflects the child's protection. A child's record might indicate administration of MMR vaccine when only single-antigen measles vaccine was administered. A study of children adopted from the People's Republic of China, Russia, and Eastern Europe determined that only 39% (range: 17%--88% by country) of children with documentation of >3 doses of DTP before adoption had protective levels of diphtheria and tetanus antitoxin (142). However, antibody testing was performed by using a hemagglutination assay, which tends to underestimate protection and cannot directly be compared with antibody concentration (143). Another study measured antibody to diphtheria and tetanus toxins among 51 children who had records of having received >2 doses of DTP. The majority of the children were from Russia, Eastern Europe, and Asian countries, and 78% had received all their vaccine doses in an orphanage. Overall, 94% had evidence of protection against diphtheria (EIA > 0.1 IU/mL). A total of 84% had protection against tetanus (enzyme-linked immunosorbent assay [ELISA] > 0.5 IU/mL). Among children without protective tetanus antitoxin concentration, all except one had records of >3 doses of vaccine, and the majority of nonprotective concentrations were categorized as indeterminate (ELISA = 0.05--0.49 IU/mL) (144). Reasons for the discrepant findings in these two studies probably relate to different laboratory methodologies; the study using a hemagglutination assay might have underestimated the number of children who were protected. Additional studies using standardized methodologies are needed. Data are likely to remain limited for countries other than the People's Republic of China, Russia, and Eastern Europe because of the limited number of adoptees from other countries.
Physicians and other health-care providers can follow one of multiple approaches if a question exists regarding whether vaccines administered to an international adoptee were immunogenic. Repeating the vaccinations is an acceptable option. Doing so is usually safe and avoids the need to obtain and interpret serologic tests. If avoiding unnecessary injections is desired, judicious use of serologic testing might be helpful in determining which immunizations are needed. This report provides guidance on possible approaches to evaluation and revaccination for each vaccine recommended universally for children in the United States (see Table 6 and the following sections).
MMR Vaccine
The simplest approach to resolving concerns regarding MMR immunization among internationally adopted children is to revaccinate with one or two doses of MMR vaccine, depending on the child's age. Serious adverse events after MMR vaccinations are rare (6). No evidence indicates that administering MMR vaccine increases the risk for adverse reactions among persons who are already immune to measles, mumps, or rubella as a result of previous vaccination or natural disease. Doses of measles-containing vaccine administered before the first birthday should not be counted as part of the series (6). Alternatively, serologic testing for immunoglobulin G (IgG) antibody to vaccine viruses indicated on the vaccination record can be considered. Serologic testing is widely available for measles and rubella IgG antibody. A child whose record indicates receipt of monovalent measles or measles-rubella vaccine at age >1 year and who has protective antibody against measles and rubella should receive a single dose of MMR as age-appropriate to ensure protection against mumps (and rubella if measles vaccine alone had been used). If a child whose record indicates receipt of MMR at age >12 months has a protective concentration of antibody to measles, no additional vaccination is needed unless required for school entry.
Hib Vaccine
Serologic correlates of protection for children vaccinated >2 months previously might be difficult to interpret. Because the number of vaccinations needed for protection decreases with age and adverse events are rare (24), age-appropriate vaccination should be provided. Hib vaccination is not recommended routinely for children aged >5 years.
Hepatitis B Vaccine
Serologic testing for HBsAg is recommended for international adoptees, and children determined to be HBsAg-positive should be monitored for the development of liver disease. Household members of HBsAg-positive children should be vaccinated. A child whose records indicate receipt of >3 doses of vaccine can be considered protected, and additional doses are not needed if >1 doses were administered at age >6 months. Children who received their last hepatitis B vaccine dose at age <6 months should receive an additional dose at age >6 months. Those who have received <3 doses should complete the series at the recommended intervals and ages (Table 1).
Poliovirus Vaccine
The simplest approach is to revaccinate internationally adopted children with IPV according to the U.S. schedule. Adverse events after IPV are rare (4). Children appropriately vaccinated with three doses of OPV in economically developing countries might have suboptimal seroconversion, including to type 3 poliovirus (125). Serologic testing for neutralizing antibody to poliovirus types 1, 2, and 3 can be obtained commercially and at certain state health department laboratories. Children with protective titers against all three types do not need revaccination and should complete the schedule as age-appropriate. Alternately, because the booster response after a single dose of IPV is excellent among children who previously received OPV (3), a single dose of IPV can be administered initially with serologic testing performed 1 month later.
DTaP Vaccine
Vaccination providers can revaccinate a child with DTaP vaccine without regard to recorded doses; however, one concern regarding this approach is that data indicate increased rates of local adverse reactions after the fourth and fifth doses of DTP or DTaP (42). If a revaccination approach is adopted and a severe local reaction occurs, serologic testing for specific IgG antibody to tetanus and diphtheria toxins can be measured before administering additional doses. Protective concentration** indicates that further doses are unnecessary and subsequent vaccination should occur as age-appropriate. No established serologic correlates exist for protection against pertussis.
For a child whose record indicates receipt of >3 doses of DTP or DTaP, serologic testing for specific IgG antibody to both diphtheria and tetanus toxin before additional doses is a reasonable approach. If a protective concentration is present, recorded doses can be considered valid, and the vaccination series should be completed as age-appropriate. Indeterminate antibody concentration might indicate immunologic memory but antibody waning; serology can be repeated after a booster dose if the vaccination provider wishes to avoid revaccination with a complete series.
Alternately, for a child whose records indicate receipt of >3 doses, a single booster dose can be administered, followed by serologic testing after 1 month for specific IgG antibody to both diphtheria and tetanus toxins. If a protective concentration is obtained, the recorded doses can be considered valid and the vaccination series completed as age-appropriate. Children with indeterminate concentration after a booster dose should be revaccinated with a complete series.
Varicella Vaccine
Varicella vaccine is not administered in the majority of countries. A child who lacks a reliable medical history regarding prior varicella disease should be vaccinated as age-appropriate (8).
Pneumococcal Vaccines
Pneumococcal conjugate and pneumococcal polysaccharide vaccines are not administered in the majority of countries and should be administered as age-appropriate or as indicated by the presence of underlying medical conditions (26,43).
Altered Immunocompetence
ACIP's statement regarding vaccinating immunocompromised persons summarizes recommendations regarding the efficacy, safety, and use of specific vaccines and immune globulin preparations for immunocompromised persons (145). ACIP statements regarding individual vaccines or immune globulins contain additional information regarding those concerns.
Severe immunosuppression can be the result of congenital immunodeficiency, HIV infection, leukemia, lymphoma, generalized malignancy or therapy with alkylating agents, antimetabolites, radiation, or a high dose, prolonged course of corticosteroids. The degree to which a person is immunocompromised should be determined by a physician. Severe complications have followed vaccination with live-virus vaccines and live bacterial vaccines among immunocompromised patients (146--153). These patients should not receive live vaccines except in certain circumstances that are noted in the following paragraphs. MMR vaccine viruses are not transmitted to contacts, and transmission of varicella vaccine virus is rare (6,138). MMR and varicella vaccines should be administered to susceptible household and other close contacts of immunocompromised patients when indicated.
Persons with HIV infection are at increased risk for severe complications if infected with measles. No severe or unusual adverse events have been reported after measles vaccination among HIV-infected persons who did not have evidence of severe immunosuppression (154--157). As a result, MMR vaccination is recommended for all HIV-infected persons who do not have evidence of severe immunosuppression†† and for whom measles vaccination would otherwise be indicated.
Children with HIV infection are at increased risk for complications of primary varicella and for herpes zoster, compared with immunocompetent children (138,158). Limited data among asymptomatic or mildly symptomatic HIV-infected children (CDC class N1 or A1, age-specific CD4+ lymphocyte percentages of >25%) indicate that varicella vaccine is immunogenic, effective, and safe (138,159). Varicella vaccine should be considered for asymptomatic or mildly symptomatic HIV-infected children in CDC class N1 or A1 with age-specific CD4+ T lymphocyte percentages of >25%. Eligible children should receive two doses of varicella vaccine with a 3-month interval between doses (138).
HIV-infected persons who are receiving regular doses of IGIV might not respond to varicella vaccine or MMR or its individual component vaccines because of the continued presence of passively acquired antibody. However, because of the potential benefit, measles vaccination should be considered approximately 2 weeks before the next scheduled dose of IGIV (if not otherwise contraindicated), although an optimal immune response is unlikely to occur. Unless serologic testing indicates that specific antibodies have been produced, vaccination should be repeated (if not otherwise contraindicated) after the recommended interval (Table 4). An additional dose of IGIV should be considered for persons on maintenance IGIV therapy who are exposed to measles >3 weeks after administering a standard dose (100--400 mg/kg body weight) of IGIV.
Persons with cellular immunodeficiency should not receive varicella vaccine. However, ACIP recommends that persons with impaired humoral immunity (e.g., hypogammaglobulinemia or dysgammaglobulinemia) should be vaccinated (138,160).
Inactivated, recombinant, subunit, polysaccharide, and conjugate vaccines and toxoids can be administered to all immunocompromised patients, although response to such vaccines might be suboptimal. If indicated, all inactivated vaccines are recommended for immunocompromised persons in usual doses and schedules. In addition, pneumococcal, meningococcal, and Hib vaccines are recommended specifically for certain groups of immunocompromised patients, including those with functional or anatomic asplenia (145,161).
Except for influenza vaccine, which should be administered annually (88), vaccination during chemotherapy or radiation therapy should be avoided because antibody response is suboptimal. Patients vaccinated while receiving immunosuppressive therapy or in the 2 weeks before starting therapy should be considered unimmunized and should be revaccinated >3 months after therapy is discontinued. Patients with leukemia in remission whose chemotherapy has been terminated for >3 months can receive live-virus vaccines.
Corticosteroids
The exact amount of systemically absorbed corticosteroids and the duration of administration needed to suppress the immune system of an otherwise immunocompetent person are not well-defined. The majority of experts agree that corticosteroid therapy usually is not a contraindication to administering live-virus vaccine when it is short-term (i.e., <2 weeks); a low to moderate dose; long-term, alternate-day treatment with short-acting preparations; maintenance physiologic doses (replacement therapy); or administered topically (skin or eyes) or by intra-articular, bursal, or tendon injection (145). Although of theoretical concern, no evidence of increased severity of reactions to live vaccines has been reported among persons receiving corticosteroid therapy by aerosol, and such therapy is not a reason to delay vaccination. The immunosuppressive effects of steroid treatment vary, but the majority of clinicians consider a dose equivalent to either >2 mg/kg of body weight or a total of 20 mg/day of prednisone or equivalent for children who weigh >10 kg, when administered for >2 weeks as sufficiently immunosuppressive to raise concern regarding the safety of vaccination with live-virus vaccines (84,145). Corticosteroids used in greater than physiologic doses also can reduce the immune response to vaccines. Vaccination providers should wait >1 month after discontinuation of therapy before administering a live-virus vaccine to patients who have received high systemically absorbed doses of corticosteroids for >2 weeks.
Vaccination of Hematopoietic Stem Cell Transplant Recipients
Hematopoietic stem cell transplant (HSCT) is the infusion of hematopoietic stem cells from a donor into a patient who has received chemotherapy and often radiation, both of which are usually bone marrow ablative. HSCT is used to treat a variety of neoplastic diseases, hematologic disorders, immunodeficiency syndromes, congenital enzyme deficiencies, and autoimmune disorders. HSCT recipients can receive either their own cells (i.e., autologous HSCT) or cells from a donor other than the transplant recipient (i.e., allogeneic HSCT). The source of the transplanted stem cells can be from either a donor's bone marrow or peripheral blood or harvested from the umbilical cord of a newborn infant (162).
Antibody titers to vaccine-preventable diseases (e.g., tetanus, poliovirus, measles, mumps, rubella, and encapsulated bacteria) decline during the 1--4 years after allogeneic or autologous HSCT if the recipient is not revaccinated (163--167). HSCT recipients are at increased risk for certain vaccine-preventable diseases, including those caused by encapsulated bacteria (i.e., pneumococcal and Hib infections). As a result, HSCT recipients should be routinely revaccinated after HSCT, regardless of the source of the transplanted stem cells. Revaccination with inactivated, recombinant, subunit, polysaccharide, and Hib vaccines should begin 12 months after HSCT (162). An exception to this recommendation is for influenza vaccine, which should be administered at >6 months after HSCT and annually for the life of the recipient thereafter. MMR vaccine should be administered 24 months after transplantation if the HSCT recipient is presumed to be immunocompetent. Varicella, meningococcal, and pneumococcal conjugate vaccines are not recommended for HSCT recipients because of insufficient experience using these vaccines among HSCT recipients (162). The household and other close contacts of HSCT recipients and health-care workers who care for HSCT recipients, should be appropriately vaccinated, including against influenza, measles, and varicella. Additional details of vaccination of HSCT recipients and their contacts can be found in a specific CDC report on this topic (162).
Vaccinating Persons with Bleeding Disorders and Persons Receiving Anticoagulant Therapy
Persons with bleeding disorders (e.g., hemophilia) and persons receiving anticoagulant therapy have an increased risk for acquiring hepatitis B and at least the same risk as the general population of acquiring other vaccine-preventable diseases. However, because of the risk for hematoma formation after injections, intramuscular injections are often avoided among persons with bleeding disorders by using the subcutaneous or intradermal routes for vaccines that are administered normally by the intramuscular route. Hepatitis B vaccine administered intramuscularly to 153 persons with hemophilia by using a 23-gauge needle, followed by steady pressure to the site for 1--2 minutes, resulted in a 4% bruising rate with no patients requiring factor supplementation (168). Whether antigens that produce more local reactions (e.g., pertussis) would produce an equally low rate of bruising is unknown.
When hepatitis B or any other intramuscular vaccine is indicated for a patient with a bleeding disorder or a person receiving anticoagulant therapy, the vaccine should be administered intramuscularly if, in the opinion of a physician familiar with the patient's bleeding risk, the vaccine can be administered with reasonable safety by this route. If the patient receives antihemophilia or similar therapy, intramuscular vaccinations can be scheduled shortly after such therapy is administered. A fine needle (<23 gauge) should be used for the vaccination and firm pressure applied to the site, without rubbing, for >2 minutes. The patient or family should be instructed concerning the risk for hematoma from the injection.
Vaccination Records
Consent to Vaccinate
The National Childhood Vaccine Injury Act of 1986 (42 U.S.C. § 300aa-26) requires that all health-care providers in the United States who administer any vaccine covered by the act§§ must provide a copy of the relevant, current edition of the vaccine information materials that have been produced by CDC before administering each dose of the vaccine. The vaccine information material must be provided to the parent or legal representative of any child or to any adult to whom the physician or other health-care provider intends to administer the vaccine. The Act does not require that a signature be obtained, but documentation of consent is recommended or required by certain state or local authorities.
Provider Records
Documentation of patient vaccinations helps ensure that persons in need of a vaccine receive it and that adequately vaccinated patients are not overimmunized, possibly increasing the risk for local adverse events (e.g., tetanus toxoid). Serologic test results for vaccine-preventable diseases (e.g., those for rubella screening) as well as documented episodes of adverse events also should be recorded in the permanent medical record of the vaccine recipient.
Health-care providers who administer vaccines covered by the National Childhood Vaccine Injury Act are required to ensure that the permanent medical record of the recipient (or a permanent office log or file) indicates the date the vaccine was administered, the vaccine manufacturer, the vaccine lot number, and the name, address, and title of the person administering the vaccine. Additionally, the provider is required to record the edition date of the vaccine information materials distributed and the date those materials were provided. Regarding this Act, the term health-care provider is defined as any licensed health-care professional, organization, or institution, whether private or public (including federal, state, and local departments and agencies), under whose authority a specified vaccine is administered. ACIP recommends that this same information be kept for all vaccines, not just for those required by the National Childhood Vaccine Injury Act.
Patients' Personal Records
Official immunization cards have been adopted by every state, territory, and the District of Columbia to encourage uniformity of records and to facilitate assessment of immunization status by schools and child care centers. The records also are key tools in immunization education programs aimed at increasing parental and patient awareness of the need for vaccines. A permanent immunization record card should be established for each newborn infant and maintained by the parent or guardian. In certain states, these cards are distributed to new mothers before discharge from the hospital. Using immunization record cards for adolescents and adults also is encouraged.
Registries
Immunization registries are confidential, population-based, computerized information systems that collect vaccination data for as many children as possible within a geographic area. Registries are a critical tool that can increase and sustain increased vaccination coverage by consolidating vaccination records of children from multiple providers, generating reminder and recall vaccination notices for each child, and providing official vaccination forms and vaccination coverage assessments (169). A fully operational immunization registry also can prevent duplicate vaccinations, limit missed appointments, reduce vaccine waste, and reduce staff time required to produce or locate immunization records or certificates. The National Vaccine Advisory Committee strongly encourages development of community- or state-based immunization registry systems and recommends that vaccination providers participate in these registries whenever possible (170,171). A 95% participation of children aged <6 years in fully operational population-based immunization registries is a national health objective for 2010 (172).
Reporting Adverse Events After Vaccination
Modern vaccines are safe and effective; however, adverse events have been reported after administration of all vaccines (82). These events range from frequent, minor, local reactions to extremely rare, severe, systemic illness (e.g., encephalopathy). Establishing evidence for cause-and-effect relationships on the basis of case reports and case series alone is impossible because temporal association alone does not necessarily indicate causation. Unless the syndrome that occurs after vaccination is clinically or pathologically distinctive, more detailed epidemiologic studies to compare the incidence of the event among vaccinees with the incidence among unvaccinated persons are often necessary. Reporting adverse events to public health authorities, including serious events, is a key stimulus to developing studies to confirm or refute a causal association with vaccination. More complete information regarding adverse reactions to a specific vaccine can be found in the ACIP recommendations for that vaccine and in a specific statement on vaccine adverse reactions (82).
The National Childhood Vaccine Injury Act requires health-care providers to report selected events occurring after vaccination to the Vaccine Adverse Event Reporting System (VAERS). Events for which reporting is required appear in the Vaccine Injury Table.¶¶ Persons other than health-care workers also can report adverse events to VAERS. Adverse events other than those that must be reported or that occur after administration of vaccines not covered by the act, including events that are serious or unusual, also should be reported to VAERS, even if the physician or other health-care provider is uncertain they are related causally. VAERS forms and instructions are available in the FDA Drug Bulletin, by calling the 24-hour VAERS Hotline at 800-822-7967, or from the VAERS website at http://www.vaers.org (accessed November 7, 2001).
Vaccine Injury Compensation Program
The National Vaccine Injury Compensation Program, established by the National Childhood Vaccine Injury Act, is a no-fault system in which persons thought to have suffered an injury or death as a result of administration of a covered vaccine can seek compensation. The program, which became operational on October 1, 1988, is intended as an alternative to civil litigation under the traditional tort system in that negligence need not be proven. Claims arising from covered vaccines must first be adjudicated through the program before civil litigation can be pursued.
The program relies on a Vaccine Injury Table listing the vaccines covered by the program as well as the injuries, disabilities, illnesses, and conditions (including death) for which compensation might be awarded. The table defines the time during which the first symptom or substantial aggravation of an injury must appear after vaccination. Successful claimants receive a legal presumption of causation if a condition listed in the table is proven, thus avoiding the need to prove actual causation in an individual case. Claimants also can prevail for conditions not listed in the table if they prove causation. Injuries after administration of vaccines not listed in the legislation authorizing the program are not eligible for compensation through the program. Additional information is available from the following:
Benefit and Risk Communication
Parents, guardians, legal representatives, and adolescent and adult patients should be informed regarding the benefits and risks of vaccines in understandable language. Opportunity for questions should be provided before each vaccination. Discussion of the benefits and risks of vaccination is sound medical practice and is required by law.
The National Childhood Vaccine Injury Act requires that vaccine information materials be developed for each vaccine covered by the Act. These materials, known as Vaccine Information Statements, must be provided by all public and private vaccination providers each time a vaccine is administered. Copies of Vaccine Information Statements are available from state health authorities responsible for immunization, or they can be obtained from CDC's National Immunization Program website at http://www.cdc.gov/nip (accessed November 7, 2001). Translations of Vaccine Information Statements into languages other than English are available from certain state immunization programs and from the Immunization Action Coalition website at http://www.immunize.org (accessed November 7, 2001).
Health-care providers should anticipate that certain parents or patients will question the need for or safety of vaccination, refuse certain vaccines, or even reject all vaccinations. A limited number of persons might have religious or personal objections to vaccinations. Others wish to enter into a dialogue regarding the risks and benefits of certain vaccines. Having a basic understanding of how patients view vaccine risk and developing effective approaches in dealing with vaccine safety concerns when they arise is imperative for vaccination providers.
Each person understands and reacts to vaccine information on the basis of different factors, including prior experience, education, personal values, method of data presentation, perceptions of the risk for disease, perceived ability to control those risks, and their risk preference. Increasingly, through the media and nonauthoritative Internet sites, decisions regarding risk are based on inaccurate information. Only through direct dialogue with parents and by using available resources, health-care professionals can prevent acceptance of media reports and information from nonauthoritative Internet sites as scientific fact.
When a parent or patient initiates discussion regarding a vaccine controversy, the health-care professional should discuss the specific concerns and provide factual information, using language that is appropriate. Effective, empathetic vaccine risk communication is essential in responding to misinformation and concerns, although recognizing that for certain persons, risk assessment and decision-making is difficult and confusing. Certain vaccines might be acceptable to the resistant parent. Their concerns should then be addressed in the context of this information, using the Vaccine Information Statements and offering other resource materials (e.g., information available on the National Immunization Program website).
Although a limited number of providers might choose to exclude from their practice those patients who question or refuse vaccination, the more effective public health strategy is to identify common ground and discuss measures that need to be followed if the patient's decision is to defer vaccination. Health-care providers can reinforce key points regarding each vaccine, including safety, and emphasize risks encountered by unimmunized children. Parents should be advised of state laws pertaining to school or child care entry, which might require that unimmunized children stay home from school during outbreaks. Documentation of these discussions in the patient's record, including the refusal to receive certain vaccines (i.e., informed refusal), might reduce any potential liability if a vaccine-preventable disease occurs in the unimmunized patient.
Vaccination Programs
The best way to reduce vaccine-preventable diseases is to have a highly immune population. Universal vaccination is a critical part of quality health care and should be accomplished through routine and intensive vaccination programs implemented in physicians' offices and in public health clinics. Programs should be established and maintained in all communities to ensure vaccination of all children at the recommended age. In addition, appropriate vaccinations should be available for all adolescents and adults.
Physicians and other pediatric vaccination providers should adhere to the standards for child and adolescent immunization practices (1). These standards define appropriate vaccination practices for both the public and private sectors. The standards provide guidance on practices that will result in eliminating barriers to vaccination. These include practices aimed at eliminating unnecessary prerequisites for receiving vaccinations, eliminating missed opportunities to vaccinate, improving procedures to assess vaccination needs, enhancing knowledge regarding vaccinations among parents and providers, and improving the management and reporting of adverse events. Additionally, the standards address the importance of recall and reminder systems and using assessments to monitor clinic or office vaccination coverage levels among patients.
Standards of practice also have been published to increase vaccination coverage among adults (2). Persons aged >65 years and all adults with medical conditions that place them at risk for pneumococcal disease should receive >1 doses of pneumococcal polysaccharide vaccine. All persons aged >50 years and those with medical conditions that increase the risk for complications from influenza should receive annual influenza vaccination. All adults should complete a primary series of tetanus and diphtheria toxoids and receive a booster dose every 10 years. Adult vaccination programs also should provide MMR and varicella vaccines whenever possible to anyone susceptible to measles, mumps, rubella, or varicella. Persons born after 1956 who are attending college (or other posthigh school educational institutions), who are employed in environments that place them at increased risk for measles transmission (e.g., health-care facilities), or who are traveling to areas with endemic measles, should have documentation of having received two doses of MMR on or after their first birthday or other evidence of immunity (6,173). All other adults born after 1956 should have documentation of >1 doses of MMR vaccine on or after their first birthday or have other evidence of immunity. No evidence indicates that administering MMR vaccine increases the risk for adverse reactions among persons who are already immune to measles, mumps, or rubella as a result of previous vaccination or disease. Widespread use of hepatitis B vaccine is encouraged for all persons who might be at increased risk (e.g., adolescents and adults who are either in a group at high risk or reside in areas with increased rates of injection-drug use, teenage pregnancy, or sexually transmitted disease).
Every visit to a physician or other health-care provider can be an opportunity to update a patient's immunization status with needed vaccinations. Official health agencies should take necessary steps, including developing and enforcing school immunization requirements, to ensure that students at all grade levels (including college) and those in child care centers are protected against vaccine-preventable diseases. Agencies also should encourage institutions (e.g., hospitals and long-term care facilities) to adopt policies regarding the appropriate vaccination of patients, residents, and employees (173).
Dates of vaccination (day, month, and year) should be recorded on institutional immunization records (e.g., those kept in schools and child care centers). This record will facilitate assessments that a primary vaccination series has been completed according to an appropriate schedule and that needed booster doses have been administered at the appropriate time.
The independent, nonfederal Task Force on Community Preventive Services (the Task Force) gives public health decision-makers recommendations on population-based interventions to promote health and prevent disease, injury, disability, and premature death. The recommendations are based on systematic reviews of the scientific literature regarding effectiveness and cost-effectiveness of these interventions. In addition, the Task Force identifies critical information regarding the other effects of these interventions, as well as the applicability to specific populations and settings and the potential barriers to implementation. This information is available through the Internet at http://www.thecommunityguide.org (accessed November 7, 2001).
Beginning in 1996, the Task Force systematically reviewed published evidence on the effectiveness and cost-effectiveness of population-based interventions to increase coverage of vaccines recommended for routine use among children, adolescents, and adults. A total of 197 articles were identified that evaluated a relevant intervention, met inclusion criteria, and were published during 1980--1997. Reviews of 17 specific interventions were published in 1999 (174--176). Using the results of their review, the Task Force made recommendations regarding the use of these interventions (177). A number of interventions were identified and recommended on the basis of published evidence. The interventions and the recommendations are summarized in this report (Table 7).
Vaccine Information Sources
In addition to these general recommendations, other sources are available that contain specific and updated vaccine information.
National Immunization Information Hotline
The National Immunization Information Hotline is supported by CDC's National Immunization Program and provides vaccination information for health-care providers and the public, 8:00 am--11:00 pm, Monday--Friday:
Telephone (English): 800-232-2522
Telephone (Spanish): 800-232-0233
Telephone (TTY): 800-243-7889
Internet: http://www.ashastd.org (accessed November 7, 2001)
CDC's National Immunization Program
CDC's National Immunization Program website provides direct access to immunization recommendations of the Advisory Committee on Immunization Practices (ACIP), vaccination schedules, vaccine safety information, publications, provider education and training, and links to other immunization-related websites. It is located at http://www.cdc.gov/nip (accessed November 7, 2001).
Morbidity and Mortality Weekly Report
ACIP recommendations regarding vaccine use, statements of vaccine policy as they are developed, and reports of specific disease activity are published by CDC in the Morbidity and Mortality Weekly Report (MMWR) series. Electronic subscriptions are free and available at http://www.cdc.gov/subscribe.html (accessed November 7, 2001). Printed subscriptions are available at
Superintendent of Documents
U.S. Government Printing Office
Washington, D.C. 20402-9235
American Academy of Pediatrics (AAP)
Every 3 years, AAP issues the Red Book: Report of the Committee on Infectious Diseases, which contains a composite summary of AAP recommendations concerning infectious diseases and immunizations for infants, children, and adolescents.
Telephone: 888-227-1770
Internet: http://www.aap.org (accessed November 7, 2001)
American Academy of Family Physicians (AAFP)
Information from the professional organization of family physicians is available at http://www.aafp.org (accessed November 7, 2001).
Immunization Action Coalition
This source provides extensive free provider and patient information, including translations of Vaccine Information Statements into multiple languages. The Internet address is http://www.immunize.org (accessed November 7, 2001).
National Network for Immunization Information
This information source is provided by the Infectious Diseases Society of America, Pediatric Infectious Diseases Society, AAP, American Nurses Association, and other professional organizations. It provides objective, science-based information regarding vaccines for the public and providers. The Internet site is http://www.immunizationinfo.org (accessed November 7, 2001).
Vaccine Education Center
Located at the Children's Hospital of Philadelphia, this source provides patient and provider information. The Internet address is http://www.vaccine.chop.edu (accessed November 7, 2001).
Institute for Vaccine Safety
Located at Johns Hopkins University School of Public Health, this source provides information regarding vaccine safety concerns and objective and timely information to health-care providers and parents. It is available at http://www.vaccinesafety.edu (accessed November 7, 2001).
National Partnership for Immunization
This national organization encourages greater acceptance and use of vaccinations for all ages through partnerships with public and private organizations. Their Internet address is http://www.partnersforimmunization.org (accessed November 7, 2001).
State and Local Health Departments
State and local health departments provide technical advice through hotlines, electronic mail, and Internet sites, including printed information regarding vaccines and immunization schedules, posters, and other educational materials.
Acknowledgments
The members of the Advisory Committee on Immunization Practices are grateful for the contributions of Margaret Hostetter, M.D., Yale Child Health Research Center; Mary Staat, M.D., Children's Hospital Medical Center of Cincinnati; Deborah Wexler, M.D., Immunization Action Coalition; and John Grabenstein, Ph.D., U.S. Army Medical Command.
References
176 Briss PA, Rodewald LE, Hinman AR, et al. and the Task Force on Community Preventive Services. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prev Med 2000;18(1 Suppl):97--140.
* During measles outbreaks, if cases are occurring among infants aged <12 months, measles vaccination of infants as young as 6 months can be undertaken as an outbreak control measure. However, doses administered at ages <12 months should not be counted as part of the series (Source: CDC. Measles, mumps, and rubella vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices [ACIP]. MMWR 1998;47[No. RR-8]:157).
†
In certain situations, local or state requirements might mandate that doses of selected vaccines be administered on or after specific ages. For example, a school entry requirement might not accept a dose of MMR or varicella vaccine administered before the child's first birthday. ACIP recommends that physicians and other health-care providers comply with local or state vaccination requirements when scheduling and administering vaccines.§
The exception is the two-dose hepatitis B vaccination series for adolescents aged 1115 years. Only Recombivax HB® (Merck Vaccine Division) should be used in this schedule. Engerix-B® is not approved by FDA for this schedule.¶
Internet sites with device listings are identified for information purposes only. CDC, the U.S. Public Health Service, and the Department of Health and Human Services do not endorse any specific device or imply that the devices listed would all satisfy the needle-stick prevention regulations.** Toxin neutralization testing is reliable but not readily available. Enzyme immunoassay tests are the most readily available, although passive hemagglutination is available in certain areas. Physicians should contact the laboratory performing the test for interpretive standards and limitations. Protective concentrations for diphtheria are defined as >0.1 IU/mL and for tetanus as >0.10.2 IU/mL.
††
As defined by a low age-specific total CD4+ T lymphocyte count or a low CD4+ T lymphocyte count as a percentage of total lymphocytes. ACIP recommendations for using MMR vaccine contain additional details regarding the criteria for severe immunosuppression in persons with HIV infection (Source: CDC. Measles, mumps, and rubella vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices [ACIP]. MMWR 1998;47[No. RR-8]:157).§§
As of January 2002, vaccines covered by the act include diphtheria, tetanus, pertussis, measles, mumps, rubella, poliovirus, hepatitis B, Hib, varicella, and pneumococcal conjugate.¶¶
The Vaccine Injury Table can be obtained from the Vaccine Injury Compensation Program Internet site at <http://www.hrsa.dhhs.gov/bhpr/vicp/table.htm> (accessed November 7, 2001).*** Standards for pediatric, adolescent, and adult immunization practices are being revised and will be posted on CDC's National Immunization Program Interne site (
http://www.cdc.gov/nip; accessed November 7, 2001) as soon as the updates are available.
Abbreviations Used in This Publication
AAFP
American Academy of Family Physicians
AAP
American Academy of Pediatrics
ACIP
Advisory Committee on Immunization Practices
DT
pediatric diphtheria-tetanus toxoid
DTaP
diphtheria and tetanus toxoids and acellular pertussis vaccine
DTP
diphtheria and tetanus toxoids and whole-cell pertussis vaccine
EIA/ELISA
enzyme immunoassay
FDA
Food and Drug Administration
GBS
Guillain-Barré syndrome
HBIG
hepatitis B immune globulin
HbOC
diphtheria CRM197 (CRM, cross-reactive material) protein conjugate
HBsAg
hepatitis B surface antigen
Hib
Haemophilus influenzae type b
HIV
human immunodeficiency virus
HSCT
hematopoietic stem cell transplant
IgG
immunoglobulin G
IGIV
intravenous immune globulin
IPV
inactivated poliovirus vaccine
JIs
jet injectors
MMR
measles, mumps, rubella vaccine
OPV
oral poliovirus vaccine
OSHA
Occupational Safety and Health Administration
PCV
pneumococcal conjugate vaccine
PPD
purified protein derivative
PRP-OMP
polyribosylribitol phosphate-meningococcal outer membrane protein
PRP-T
PRP-tetanus
PPV
pneumococcal polysaccharide vaccine
Td
adult tetanus-diphtheria toxoid
VAERS
Vaccine Adverse Event Reporting System
VAPP
vaccine-associated paralytic polio
Definitions Used in This Report
Adverse event. An untoward event that occurs after a vaccination that might be caused by the vaccine product or vaccination process. It includes events that are 1) vaccine-induced: caused by the intrinsic characteristic of the vaccine preparation and the individual response of the vaccinee; these events would not have occurred without vaccination (e.g., vaccine-associated paralytic poliomyelitis); 2) vaccine-potentiated: would have occurred anyway, but were precipitated by the vaccination (e.g., first febrile seizure in a predisposed child); 3) programmatic error: caused by technical errors in vaccine preparation, handling, or administration; 4) coincidental: associated temporally with vaccination by chance or caused by underlying illness. Special studies are needed to determine if an adverse event is a reaction or the result of another cause (Sources: Chen RT. Special methodological issues in pharmacoepidemiology studies of vaccine safety. In: Strom BL, ed. Pharmacoepidemiology. 3rd ed. Sussex, England: John Wiley & Sons, 2000:707--32; and Fenichel GM, Lane DA, Livengood JR, Horwitz SJ, Menkes JH, Schwartz JF. Adverse events following immunization: assessing probability of causation. Pediatr Neurol 1989;5:287--90).
Adverse reaction. An undesirable medical condition that has been demonstrated to be caused by a vaccine. Evidence for the causal relationship is usually obtained through randomized clinical trials, controlled epidemiologic studies, isolation of the vaccine strain from the pathogenic site, or recurrence of the condition with repeated vaccination (i.e., rechallenge); synonyms include side effect and adverse effect).
Immunobiologic. Antigenic substances (e.g., vaccines and toxoids) or antibody-containing preparations (e.g., globulins and antitoxins) from human or animal donors. These products are used for active or passive immunization or therapy. The following are examples of immunobiologics:
Vaccine. A suspension of live (usually attenuated) or inactivated microorganisms (e.g., bacteria or viruses) or fractions thereof administered to induce immunity and prevent infectious disease or its sequelae. Some vaccines contain highly defined antigens (e.g., the polysaccharide of Haemophilus influenzae type b or the surface antigen of hepatitis B); others have antigens that are complex or incompletely defined (e.g., killed Bordetella pertussis or live attenuated viruses).
Toxoid. A modified bacterial toxin that has been made nontoxic, but retains the ability to stimulate the formation of antibodies to the toxin.
Immune globulin. A sterile solution containing antibodies, which are usually obtained from human blood. It is obtained by cold ethanol fractionation of large pools of blood plasma and contains 15%--18% protein. Intended for intramuscular administration, immune globulin is primarily indicated for routine maintenance of immunity among certain immunodeficient persons and for passive protection against measles and hepatitis A.
Intravenous immune globulin. A product derived from blood plasma from a donor pool similar to the immune globulin pool, but prepared so that it is suitable for intravenous use. Intravenous immune globulin is used primarily for replacement therapy in primary antibody-deficiency disorders, for treatment of Kawasaki disease, immune thrombocytopenic purpura, hypogammaglobulinemia in chronic lymphocytic leukemia, and certain cases of human immunodeficiency virus infection (Table 2).
Hyperimmune globulin (specific). Special preparations obtained from blood plasma from donor pools preselected for a high antibody content against a specific antigen (e.g., hepatitis B immune globulin, varicella-zoster immune globulin, rabies immune globulin, tetanus immune globulin, vaccinia immune globulin, cytomegalovirus immune globulin, respiratory syncytial virus immune globulin, botulism immune globulin).
Monoclonal antibody. An antibody product prepared from a single lymphocyte clone, which contains only antibody against a single microorganism.
Antitoxin. A solution of antibodies against a toxin. Antitoxin can be derived from either human (e.g., tetanus antitoxin) or animal (usually equine) sources (e.g., diphtheria and botulism antitoxin). Antitoxins are used to confer passive immunity and for treatment.
Vaccination and Immunization. The terms vaccine and vaccination are derived from vacca, the Latin term for cow. Vaccine was the term used by Edward Jenner to describe material used (i.e., cowpox virus) to produce immunity to smallpox. The term vaccination was used by Louis Pasteur in the 19th century to include the physical act of administering any vaccine or toxoid. Immunization is a more inclusive term, denoting the process of inducing or providing immunity by administering an immunobiologic. Immunization can be active or passive. Active immunization is the production of antibody or other immune responses through administration of a vaccine or toxoid. Passive immunization means the provision of temporary immunity by the administration of preformed antibodies. Four types of immunobiologics are administered for passive immunization: 1) pooled human immune globulin or intravenous immune globulin, 2) hyperimmune globulin (specific) preparations, 3) monoclonal antibody preparations, and 4) antitoxins from nonhuman sources. Although persons often use the terms vaccination and immunization interchangeably in reference to active immunization, the terms are not synonymous because the administration of an immunobiologic cannot be equated automatically with development of adequate immunity.
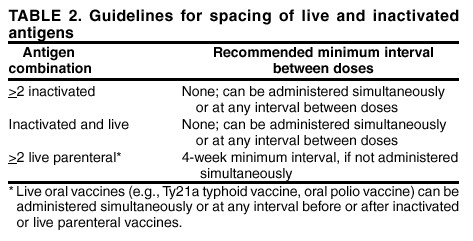
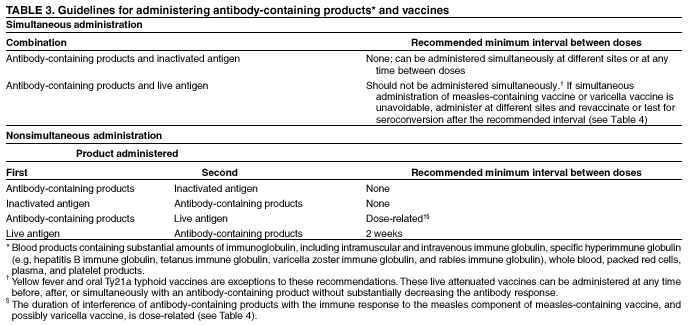
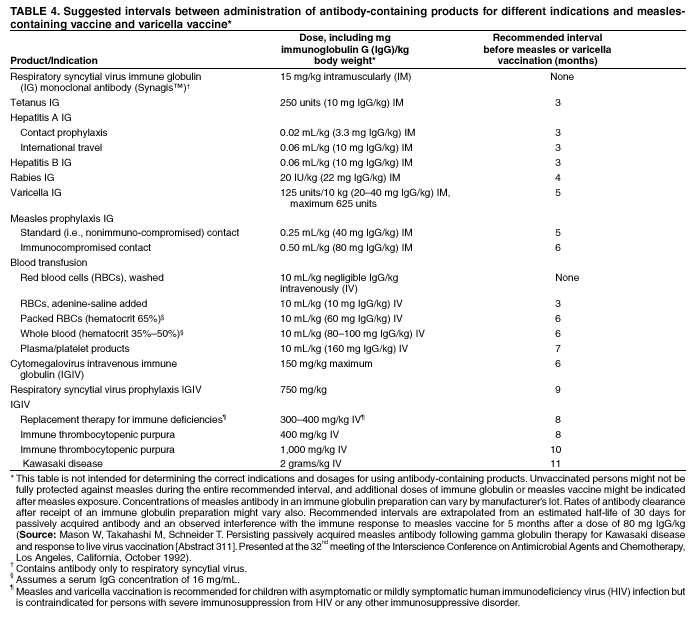
|
Advisory Committee on Immunization Practices Chairman: John F. Modlin, M.D., Professor of Pediatrics and Medicine, Dartmouth Medical School, Lebanon, New Hampshire. Executive Secretary: Dixie E. Snider, Jr., M.D., Associate Director for Science, Centers for Disease Control and Prevention, Atlanta, Georgia. Members: Dennis A. Brooks, M.D., Johnson Medical Center, Baltimore, Maryland; Richard D. Clover, M.D., University of Louisville School of Medicine, Louisville, Kentucky; Jaime Deseda-Tous, M.D., San Jorge Children's Hospital, San Juan, Puerto Rico; Charles M. Helms, M.D., Ph.D., University of Iowa Hospital and Clinics, Iowa City, Iowa ; David R. Johnson, M.D., Michigan Department of Community Health, Lansing, Michigan ; Myron J. Levin, M.D., University of Colorado School of Medicine, Denver, Colorado; Paul A. Offit, M.D., Children's Hospital of Philadelphia, Philadelphia, Pennsylvania; Margaret B. Rennels, M.D., University of Maryland School of Medicine, Baltimore, Maryland; Natalie J. Smith, M.D., California Department of Health Services, Berkeley, California; Lucy S. Tompkins, M.D., Ph.D., Stanford University Medical Center, Stanford, California; Bonnie M. Word, M.D., Monmouth Junction, New Jersey. Ex-Officio Members: James Cheek, M.D., Indian Health Service, Albuquerque, New Mexico; Carole Heilman, M.D., National Institutes of Health, Bethesda, Maryland; Karen Midthun, M.D., Food and Drug Administration, Bethesda, Maryland; Martin G. Myers, M.D., National Vaccine Program Office, Atlanta, Georgia; Kristin Lee Nichol, M.D., VA Medical Center, Minneapolis, Minnesota; Col. Benedict M. Didiega, M.D., Department of Defense, Falls Church, Virginia; Geoffrey S. Evans, M.D., Health Resources and Services Administration, Rockville, Maryland; T. Randolph Graydon, Health Care Financing Administration, Baltimore, Maryland. Liaison Representatives: American Academy of Family Physicians, Martin Mahoney, M.D., Ph.D., Clarence, New York; Richard Zimmerman, M.D., Pittsburgh, Pennsylvania; American Academy of Pediatrics, Jon Abramson, M.D., Winston-Salem, North Carolina; Gary Overturf, M.D., Albuquerque, New Mexico; American Association of Health Plans, Eric K. France, M.D., Denver, Colorado; American College of Obstetricians and Gynecologists, Stanley A. Gall, M.D., Louisville, Kentucky; American College of Physicians, Kathleen M. Neuzil, M.D., Seattle, Washington; American Hospital Association, William Schaffner, M.D., Nashville, Tennessee; American Medical Association, H. David Wilson, M.D., Grand Forks, North Dakota; Association of Teachers of Preventive Medicine, W. Paul McKinney, M.D. Louisville, Kentucky; Canadian National Advisory Committee on Immunization, Victor Marchessault, M.D., Cumberland, Ontario, Canada; Hospital Infection Control Practices Advisory Committee, Jane D. Siegel, M.D., Dallas, Texas; Infectious Diseases Society of America, Samuel L. Katz, M.D., Durham, North Carolina; London Department of Health, David M. Salisbury, M.D., London, United Kingdom; National Immunization Council and Child Health Program, Mexico, Jose Ignacio Santos, M.D., Mexico City, Mexico; National Medical Association, Rudolph E. Jackson, M.D., Atlanta, Georgia; National Vaccine Advisory Committee, Georges Peter, M.D., Providence, Rhode Island; Pharmaceutical Research and Manufacturers of America, Kevin Reilly, Radnor, Pennsylvania. Members of the General Recommendations on Immunization Working Group Advisory Committee on Immunization Practices (ACIP), Lucy Tompkins, M.D.; Chinh Le, M.D.; Richard Clover, M.D.; Natalie Smith, M.D. ACIP Liaison and Ex-Officio Members, David H. Trump, M.D., Office of the Assistant Secretary of Defense (Health Affairs); Pierce Gardner, M.D., American College of Physicians; Georges Peter, M.D., National Vaccine Advisory Committee; Victor Marchessault, M.D., Canadian National Advisory Committee on Immunization; Goeffrey Evans, M.D., Health Resources and Services Administration; Richard Zimmerman, M.D., American Academy of Family Physicians; Larry Pickering, M.D., American Academy of Pediatrics; CDC staff member, William L. Atkinson, M.D.; other members and consultants, Margaret Hostetter, M.D., Yale Child Health Research Center; Mary Staat, M.D., Children's Hospital Medical Center of Cincinnati; Deborah Wexler, M.D., Immunization Action Coalition; John Grabenstein, Ph.D., U.S. Army Medical Command; Thomas Vernon, M.D., Merck Vaccine Division; and Fredrick Ruben, M.D., Aventis-Pasteur. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.**Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov. Page converted: 2/6/2002 |