|
|
Three Cases’ Report
Authors: Maj Boguslaw, Latka Dariusz, Kita Pawel, Czerwinski Krzysztof. Institution: Department of Neurosurgery, State Medical Centre Opole, Poland Email: bmaj@wcm.opole.pl Abstract Introduction Cases Discussion Conclusions Meningioma with cystic component is not commonly encountered tumor. We report cases of three patients with cystic meningioma histologically confirmed. Tomographic images of these tumors resembled those of a glial or metastatic origin with cystic or necrotic changes and are easily confused. In a 2-year period (1997-1999) in our Department we have three patient with cystic meningioma and it is 5.4% of all patients with meningiomas we have . Key words: Computed tomography; Cystic meningioma; Extra-axial tumor. The meningioma is by far the most common extra-axial intracranial tumor, and it is also the most common primary intracranial tumor that is not of glial origin. Meningiomas are mostly solid tumors, and their charcteristic appearance in computed tomography or magnetic resonance images usually leads to correct preoperative diagnosis. Meningiomas with cystic component mimic malignant gliomas or metastatic lesions, especially intracerebral cystic meningioma may lead to misdiagnosis. We review three cases with cystic meningioma and pre- and postoperative computed tomography images. All patient recover well after surgery. CASES PRESENTATION PATIENT 1 A 63-year-old man with history of periodic headache and few week befor admition episod of absence epilepsy. Introduced computed tomography diagnosis revealed two separate extra-axial tumors in the pterional and frontal region on the left site. (Figure 1 – CT before operations with two separate tumors.) The frontal lesion acompanied by cystic component. First there was totaly removed pterional tumor. On six day after operation appeared afasia. Control tomography revealed intracystic haemorrhage of the second lesion. Frontal tumor was also totaly resectet during second operation. Hisological survey confermed atypical meningioma of both tumors. There was no tumor in afteroperations tomography. (Figure 2 – postoperative CT). Without nuerological deficit patient was dismissed seven days after surgical treatment.
Figure 2
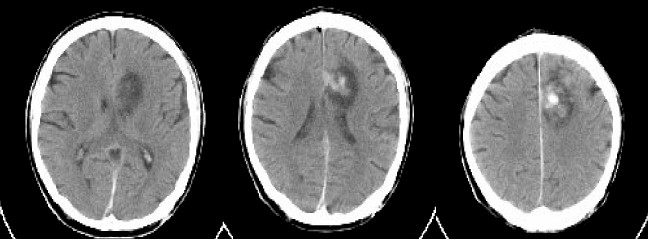
PATIENT 2 A 70-year-old man with 8-month progressive right-sided weakness and few episodes of epileptic attacks (focal epilepsy). A CT scan revealed cystic, intracerebral tumor in the left frontal lobe with cystic wall and tumor nodule marked after contrast administration. (Figure 3 without contrast and Figure 4 after contrast administration). An image strictely like astroglial tumours. Operatively, with assistance of USG the cyst was caniulated and yellowish, transparent fluid was taken. Very solid, extra-axial tumor was removed totally. In control CT we found only small amount of blood in the region (Figure 5). Patient recovered good. Dismissed on 12-day after operation. For a few months we plan him for the control CT.
Figure 4 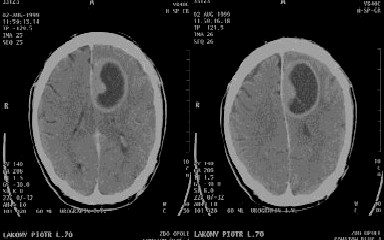
PATIENT 3 A 63-year old male patient with 4-years history of syncope end epilepsy and diagnosed on CT ’96 small, left frontoparietal meningioma qualified under observation. Without progression in repeated CT and MRI images (Figure 6-Aug’96, Figure 7-Dec’96, Figure 8-Jan’98). Two month before admission developed right hemiparesis and motor aphasia. MRI-August’99(Figure 9) compared with CT-Januarry’98(Figure 8) showed amazing development of polycystic part around the tumor with significant mass effect without increasing of the solid part of the tumor. At surgery a small solid tumor was removed totally and few cystic conpartments disclosed with delivery of cerebrospinal fluid. The most probable is that development of the cyst was due to local entrapment of CSF by the tumor and its arachnoid adhesions. Sudden clinical deterioration sure enough was provoked by the rapid expansion of the cyst volume. Histologically it was microcystic meningioma. Patient was reoperated two days later because hemorrhage into the region. He neurologically improved quickly, dismissed two weeks after operation with minimal weakness of the left extremities and decreasing aphasia. Figure 6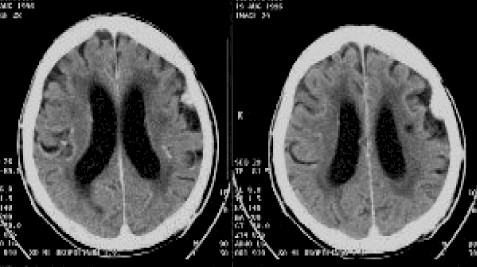
Figure 7 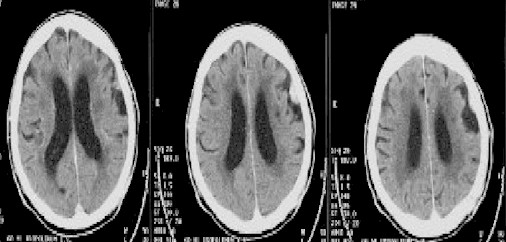
Figure 8 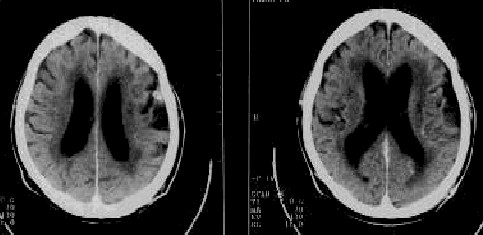
Figure 9 
Nauta classified cystic meningiomas into four types according to the site of the cavity: 1) centrally located intratumoral cyst; 2) peripherally located intratumoral cyst; 3) peritumoral cyst in the adjacent parenchyma; and 4) peritumoral cyst between the tumor and the adjacent parenchyma. Cystic meningiomas most commonly have a cyst eccentric to the tumor mass that might be Nauta Type 2 or 3, but large intratumoral cysts are rare. According to Fortuna, intratumoral cysts of Nauta Type 1, 2 are the outcome of: 1) microcystic degeneration; 2) ischemic necrosis or 3) hemorrhage. Microcystic degeneration is considered to be the confluence of the cellular degenerative phenomena such as vacuolar, myxomatous, mucoid, and fatty degeneration leading to the formation first of microcavitations and then of macrocavitations within the tumor. In addition, transudation or secretory changes within the tumor tissue may produce cysts. A peritumoral cyst of Nauta Type 3 may be the outcome of a reactive gliosis or fibroblastic proliferation or the final stage of the intense peritumoral edema. Usually, the walls of these large eccentric cysts associated with meningiomas have been composed of reactive glia or collagen; neoplastic cells have rarely been found in the distal cyst wall. The resection and careful pathological evaluation of the walls of any cyst are mandatory to avoid recurrence. This is supported by the fact that 8% of cystic meningiomas are malignant and 12% are angioblastic, probably hemangiopericytic. The formation of peritumoral cysts of Nauta Type 4 may be secondary to a widening of the subarachnoid space or mechanical trapping of the cerebrospinal fluid spaces compressed by the tumor and, less commonly, true arachnoid cysts. Rengachary recognized only two kinds of cysts: intratumoral cysts and peritumoral cysts, depending on whether the cyst is lined by meningothelial cells. In summary, pathophysiological mechanisms in the formation of meningioma cysts are ischemic central necrosis and cystic degeneration, an intratumoral hemorrhage with subsequent cystic/necrotic changes, the active secretion of fluid by functional tumor cells into the tumor, glial proliferation as a response to the presence of a tumor with the elaboration of fluid by glial cells, the evolution of peritumoral edema into a peritumoral cyst,and the loculation of cerebrospinal fluid. CONCLUSION Cystic meningioma is rare kind of tumor, in our series 5.4% of all meningioma which is comparable with literature. The most difficult is accurate preoperative diagnosis because the CT image of this tumors, especially with intratumoral cyst are easily confused with glial tumors. Wrong interpretation of CT or MRI images and incomplete extirpation of tumoral capsule could be the main factor of recurrence of the tumor.
|
To contact
Authors personally: bmaj@wcm.opole.pl |