Indice del volumen
Volume index
Comité Editorial
Editorial Board
Comité Científico
Scientific Committee
VASCULAR DEMENTIA TYPE BINSWANGER'S DISEASE IN PATIENTS WITH ACTIVE NEUROCYSTICERCOSIS.
Foyaca Sibat H, MD. Ibañez Valdés LdeF, MD.
Department of Neurology, and Department of Family Medicine University of Transkei.
Umtata. South Africa.
foyaca @ intekom.co.za
Rev Electron Biomed / Electron J Biomed 2003;1(1):32-42. pdf
Comentario de Ramón Diaz-Alersi. Hospital Puerto Real. Cadiz. España
Comentario de E. Moro-Rodríguez. Universidad Rey Juan Carlos. Facultad de Ciencias de la Salud. Madrid. España.
ABSTRACT
We report seven patients who presented with clinical manifestations of ischemic cerebrovascular disease (CVD), dementia, and on CT Scan radiological signs of active neurocysticercosis and Binswanger’s Disease (BD) were found. Two patients died due to bilateral pulmonary thromboembolism secondary to deep venous thrombosis on lower limbs and the others remain alive. In almost all of them after one day of treatment with praziquantel(PZQ) some aggravation of the clinical manifestations of BD were observed. We have hypothesized about the Taenia solium-microglial activation-coagulation disorder and glial disorders-Blood-Brain-Barrier disturbances-Binswanger’s disease. We considered that anti-parasitic therapy for active NCC in patients with an associated BD should be prescribed for some isolated cases when it’s extremely necessary.
Key Notes: Vascular Dementia, Binswanger’s disease, Neurocysticercosis, Praziquantel
INTRODUCTION
In 1550, neurocysticercosis (NCC) is described for the first time when Parandi found some rounded vesicles filled of cerebrospinal fluid (CSF) on the corpus callosum in a patient with cerebovascular disease (CVD). In 1558 Kumber provided a more detailed description of NCC from the autopsy of epileptic patient and Malpigh in 1686 nominated its as a parasitic disease and identified the parasites into the intracerebral vesicles which were named cysticercus by Laennec in XIX century.1 NCC is the most common parasitic infection of the brain caused by the larval stage (cysticercus cellulosae) of the pig tapeworm Taenia solium, affecting more than 50 million of peoples all over the world. NCC is characterized by epilepsy, intracranial hypertension, neuropsychiatry manifestation, dermatological and ocular problems, more detailed information about NCC in our region are available on-line.2 3 4 5
In 1672, the English physician Thomas Willis (1621-1672) provides the first accurate clinical observations of patients with post-stroke vascular dementia. Willis said: " I have observed in many cases that when, the Brain being indisposed, they have been distemper’d with a dullness of mind and forgetfulness, and then afterwards with a stupidity and foolishness, they would afterwards have fallen into a Palsie, which I oft did predict. For according as the places obstructed are more or less large so either a universal Palsies, or an half Palsie of one side, or else some partial resolutions of members happen".6
In 1938, Dechambre described lacunes for the first time while worked under Cruveilhier supervision at the Salpétriére Hospital in France. The word lacune (French lacune from the Latin lacuna, ae, a tiny hole, pit, or cavity) denotes a small, cystic cavity of the brain substance that usually results from an ischemic infarction in the territory of a penetrating arteriole; lacunes may follow very rarely small deep hemorrhages or an isolated giant dilation of the perivascular space.6
In 1894, Alzheimer and Binswanger described "arteriosclerotic brain atrophy", a condition characterized by "military apoplexies" or "disease foci" (lacunar infarcts) affecting the basal ganglia, internal capsule, and white matter (WM) of the Centrum ovale, associated with severe arteriosclerosis of small and large vessels.6 he also described an associated enlarged ventricles and normal cerebral cortex, Binswanger separated its from neurosyphillis and other forms of dementia in elderly peoples.7
The term état criblé (Cribiform state) and leukoaraiosis (LA) described in 1842 and 1987 respectively refers to the dilations of perivascular spaces around cerebral arterioles in the brain of elderly peoples and the radiological images of loss of density of the periventricular WM observed by computerized tomography (CT) of the brain accordingly.
In some textbook of neurology, Binswanger’s disease (BD) is described as a very uncommon disorder characterized by pseudobulbar palsy with vascular dementia due to lesions on the WM, and LA is seen on the CT Scan or MRI in third age’s patients (sixth or seventh decade). To the knowledge of those authors, about 150 cases had been reported,7
The attenuation of the subcortical WM (LA) is a hallmark of the BD. When this syndrome was described by Binswanger, he identified it as a different form of dementia (encephalitis subcorticalis chronica) with lesions of the subcortical WM "severe atheromatosis of the arteries." In 1982 Tomonaga8 reported an incidence of BD between 3 to 12 percent in the elderly. The etiology of BD is still not certain but dysfunction of the blood-brain-barrier seems to be always present.
Some of the pathological hallmark (WM lesions) of BD are also present in NCC. We had have been investigating patients with NCC and associated ischemic CVD, but unfortunately these results are still in process, however lesions of the WM in ischemic stroke does not differ from lesions on the WM in BD (WM lesions plus lacunes) although that lesions are more diffuse and prominent in BD.9
The aim of this study is to report our results from a group of patients fulfilling diagnostic criteria for BD10 (dementia-based on Mini-Mental-State, and bilateral radiological abnormalities on computed tomography), evidence of systemic vascular disease, manifestation of focal cerebrovascular disease or evidence of "subcortical" cerebral dysfunction, and NCC (Evidence of cystic lesions showing the scolex on CT)11. All of them were treated with PZQ (100 mg/kg) and prednisone (30 mg/day).
MATERIAL AND METHODS.
Seven patients diagnosed as BD and NCC were identified prospectively for the study among other patients referred to neurology clinic in Umtata General Hospital during five years period. Some of those patients presented with an associated pulmonary tuberculosis (PTB) and all of them with long-standing history of arterial hypertension. Hypertension was diagnosed according to the criteria of the World Health Organization (Geneva, Switzerland; 1985. Technical Report Series 727). Our hospital is a tertiary-care institution that offers neurological services for a rural area of about 6, 4 million peoples. Patients with stroke (defined as focal neurological deficits of acute onset, lasting more than 24 hours, due to brain ischemia as shown by CT Scan or after clinical and neuroradiological workup) were admitted to our Stroke Units (female and male) after examination in the emergency and casualty department, without further selection. Those patients were studied according to the following protocol: Detailed history of the present complaint, identification of the risk factors for stroke, and physical examination, neurological evaluation at entry and daily for the first ten days, laboratory tests, chest x-ray, electrocardiogram and hemodinamic tests, CT Scan of the brain, coagulation screen, lipid profile, and others looking for cardiovascular diseases or peripheral vasculopathies were carried out when necessary.
After the CT scan of the brain, eligible patients (n=7) had an active form of NCC without clinical signs of raised intracranial pressure.
Exclusion criteria for anti-parasitic treatment in this group included age < 59 or > 81 years, resolution of deficits within 24 hours, normal CT Scan, history of alcohol abuse (ie, > 600 g/wk), history of retarded psychomotor development, psychosis, other CNS disorder or systemic diseases known to involve the CNS, patients with severe aphasia and/or sensory impairment (blindness, deafness), severe depression and finally high suspicion of tuberculomas, pyogenic brain abscesses, mycotic granulomas, and primary or metastatic brain tumors (See the flow chart). Apart from aspirin and anticoagulant (when it was necessary), steroids medications and antiparasite treatment, other concomitant treatment was prohibited for patient while participating in the study. All patients received 100mg/kg of PZQ divided in four oral dosages of 25mg/kg each for one day only and 30 mg of prednisone daily during 4 consecutive days, and 150 mg of aspirin after breakfast. We obtained written informed consent from each patient.
Outcome measures
Response to anti-parasite treatment were assessed by neurological evaluation of the CVD disease manifestation at the baseline and one week after the anti-parasitic treatment with PZQ, and also with CT Scan of the brain a week after. All patient received the same supporting treatment and were encouraged to eat rich carbohydrate meals and the same personnel evaluated all throughout the study.
RESULTS
An experienced neurologist evaluated all patients, none patients had no previous history of any other neurological disease apart from clinical manifestations of CVD. All patients presented with elevated systolic and diastolic blood pressure ranged from 146/93mmHG to 169/114 mmHg. (Table I)
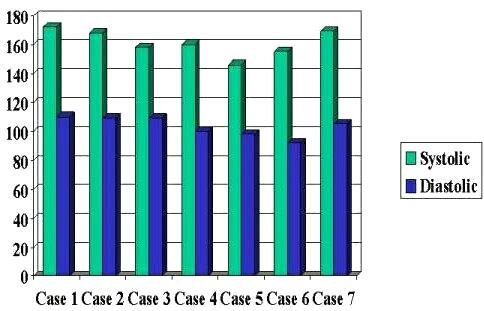
Table I. Measurement of blood pressure
Although cognitive disorder and urinary incontinence were a common clinical signs in this group; however combination of memory dysfunction, difficulty walking, and stroke in all of them were also observed (Table II).
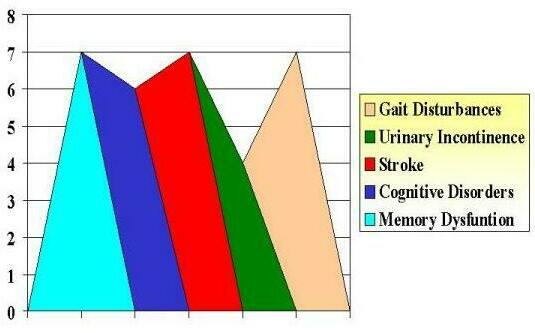
Table II. Commonest problems
Absolute criteria for NCC based on neuroimaging findings were present in all selected patients considering the cystic lesion with scolex (bright nodule within the cyst, producing the so-called "hole-with-dot" imaging) as patognomonic (Figure 1), LA was present in all patients, and lacunar infarct on the basal ganglia in six of them radiographically (Table III).
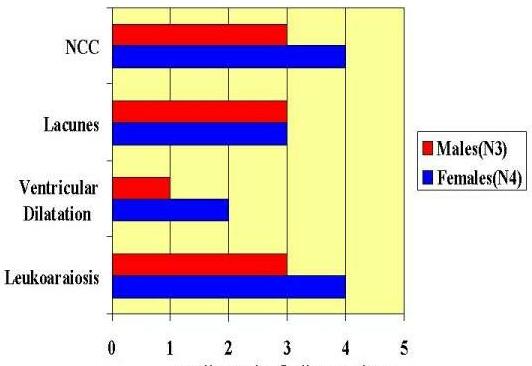
Table III. Radiography findings and sex
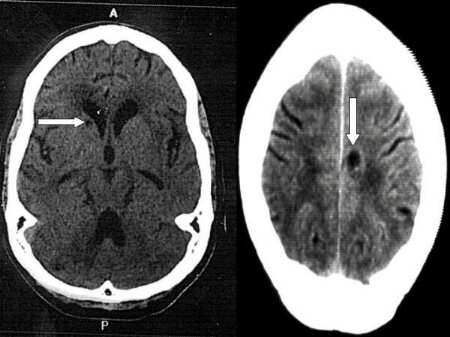
Figure 1 CT Brain Scan showing active NCC (left) and lacunar infarction on the head of the caudate nucleus (right) and leukoaraiosis
On physical examination one patient evidenced a mild improvement of gait after one single day therapy with praziquantel, one remained without remarkable changes and the other five worsened. (Table IV)
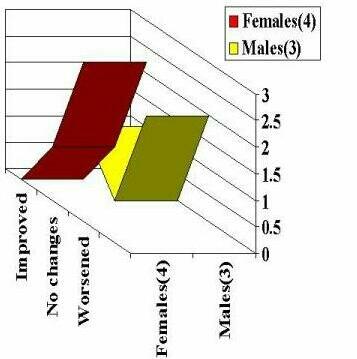
Table IV. Outcome after Praziquantel therapy
One patient developed generalized tonic-clonic epileptic attacks, other 2 died after coagulation disorders, deep venous thrombosis, massive pulmonary embolism, and ischemic hemorrhagic stroke (Figure 2) and microglial activation (Figure 3) the rest evidenced faster deterioration of the cognitive dysfunction and memory. Efficacy analysis included 7 patients (4 women and 3 man, mean age 65,17, years, range 60 to 71) treated with praziquantel/prednisone.
Patients with poorest prognosis evidenced signs of chronic arterial hypertension such as "onion-skin" changes in renal blood vessels (Figure 4)
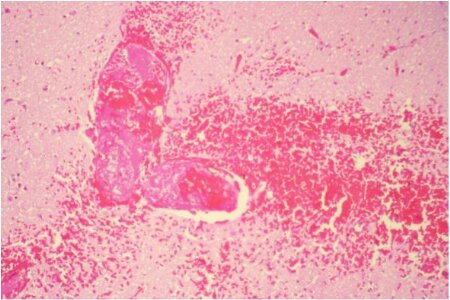
Figure 2. Thromboembolims and focal micro-haemorrhage. (15PM02 H.E.10X)

Figure 3. Microglial activation.
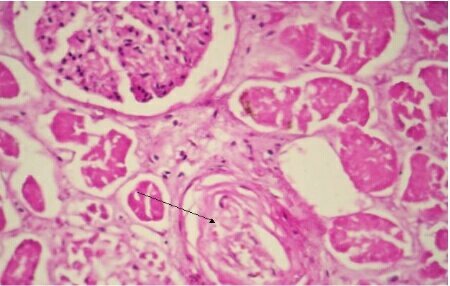
Figure 4. "Onion-skin" change in a renal blood vessel (15PM02 H.E.20X)
COMMENTS
From our personal experience BD is more common than the figure described by Gautier,7 and is characterized among other signs by subcortical neurological deficits such as gait abnormalities, rigidity, and neurogenic bladder plus psychiatry disorders including mood changes and depression, loss of memory and cognition, hypertension, evidence of systemic vascular disease or disease of the large blood vessels in the neck, stroke, blood abnormalities, and disease of the heart valves in people oldest than 60 years.
Two millions of biomedical articles are published every year, after review of some of them we found no evidence for treat all patients with NCC12 or insufficient evidence to assess whether cysticidal therapy in NCC is associated with beneficial effects (2002 Cochrane Database of Systematic Reviews)13 in other articles we found small population for the study, no radomization and double blindness, no control group, no adequate outcome measuring, wrong statitistical analysis, no inclusion or exclusion criteria, poor discussion of the results and some bioethical problems.14 15 16 17 18 19 In spite of the above-mentioned mistakes on research planning, we personally believe that some symptomatic patients without any other associated neurological disorder require anti-cysticidal therapy for NCC.
Ischaemic CVD is a relatively common but under-recognized complication of NCC usually caused by inflammatory occlusion of the arteries at the base of the brain secondary to cyiticercotic arachnoiditis, and lacunar and large infarcts have been reported20 Two of our patients die soon after treatment with PZQ for single active lesion of NCC in vesicular stage, both developed ischemic CVD and microhemorrhage were found on the necropsy, in one patient a remarkable deep venous thrombosis which did not response to heparine intravenously was confirmed. Cerebral infarction has been reported 21 22 but not in BD type, therefore from our knowledge it is a novel association no previously reported in the medical literature. Seizure disorder as complication of praziquantel therapy has been also reported,23 however we believe that seizures in our series are NCC related, rather than side effect of praziquantel, because NCC is the most common cause of acquired epilepsy worldwide and because we have been treating thousands patients with praziquantel for a long time and never ever found similar complication. Seizures also can be present as part of the clinical feature of BD. Then why it’s happened after praziquantel therapy? Well, some neurophyisiopathological events present when that parasite is dying can explain that complication. Why aggravation of cognitive dysfunction after praziquantel? First of all is good to establish that we could not distinguish patients with vascular dementia (cognitive syndrome of vascular cause) due to BD from patients with dementia due to Alzheimer Disease (AD) being it a handicap for any credible theoretical explanation. Hallmark of BD is WM lesion which can be characterized by lacunes (small infarction less than 1.5 cm in diameter, in a deep location, and without clinical evidence of significant heart disease), etat crible (cribiform or sieve-like atrophy), brain interstitial atrophy, etat lacunaire, and enecephalitis subcorticalis chronica progressiva (Binswanger’s), and "unidentified bright objects" (UBOs) on the MRI. Those lesion with hyperintensity in the periventricular WM are zones of chronic WM ischemia due to microvascular disease in the terminal zones of the medullary arteries, typically sparing the short, arcuate subcortical fibers in a pattern that has become associated with BD (partial loss of myelin sheaths and oligodendroglial cells and axon, producing a decrease of the meshwork of the WM tissue, along with mild reactive fibrillary gliosis and sparce macrophages.24 Because this finding can be seen also on the brain of elderly peoples and patient with AD we are nor considering such pathological changes as pathognomonic of BD. However senile demential of the Binswanger type is a well-defined medical condition more commonly diagnosed in centers where technique for myelin stain are used.
Although the role of alterations of the blood-brain-barrier linked to hypertensive episodes with chronic vasogenic edema in patients with BD is not well defined, the role of platelet activation as a major participant in the etiology of thromboembolic stroke is well known.
b-Thromboglobulin (BTG) is a platelet-specific protein that is released into the circulation from activated platelets, its concentration is an indicator of platelet activation in the systemic circulation and its concentration can be influenced by the presence of atherothrombotic lesions, arrhythmias, aging, renal functional impairment,25 and probable vascular lesion associated to cysticercosis. BD promote platelet-derived substances released reactions, inducing vessel wall damage and causing neuronal impairment downstream; chronic ischemia in the hemispheric white matter based on the same mechanism is aggravated in patients with NCC when the parasite is dying due to host’s immunological attack or by anti-cysiticidal drugs.
After reviewed the South Africa Medical Literature about NCC26 27 28 29 30and considering that cerebrovascular diseases is the second common cause of dementia; knowing that cerebrovascular disease is one of the complications of NCC, and that ischemic stroke during praziquantel therapy due to a secondary inflammatory vascular reaction in neurocysticercosis has been reported, 31 32 33 and finally taking in to consideration that there is insufficient evidence to determine whether cysticidal therapy is of any clinical benefit to patients with neurocysticercosis34 we consider that anti-parasitic medication against Taenia solium for patients with NCC and an associated BD, is contraindicated until proven otherwise.
REFERENCES
1.- Hernandez-Cossio O, Hernandez O. Neurocisticercosis y epilepsia en Cuba. Rev Neurol 1999;29:1003-1006.
2.- Foyaca-Sibat H, Ibañez-Valdés L de F, Awotedu A, Fernandez-Mena C. The Third International Congress of Critical Care Medicine on Internet. Nov. 2001.
http://www.uninet.edu/cimc2001/comunicaciones/foyaca/index.html
3.- Foyaca-Sibat H, Ibañez-Valdés L de F, Awotedu A, Fernandez-Mena C . Neurocysticercosis in the Former Transkei. 7th Internet World Congress for Biomedical Sciences. Inabis 2002. April 14-20, 2002 . Avaiable on-line at:
http://www.inabis2002.org/poster-congress.area-01/01011/010117.pdf
4.- Foyaca-Sibat H, Ibañez-Valdés L de F. Clinical Trial of prazinquantel and prednisone in rural patients with recurrent epileptic attacks. The Internet Journal of Neurology 2002;I(2):8-17 available on-line at: 5.- Foyaca-Sibat H. Tapeworm and the Brain. Science in Africa.2002 June XVIII. 6.- Román CR. On the History of Lacunes, Etat criblé, and the White Matter Lesions of Vascular Dementia. Cerebrovasc Dis 2002;13(suppl 2):1-6.
7.- Gautier JC, Mohr JP. Ischemic Stroke. Binswanger’s Disease. Guide to clinical neurology . Churchill Livingstone ED 1995 pag 563-564.
8.- Tomonaga M, Yamanouchi H, Tohgi H, Kameya M. Clinicopathologic study of progressive subcortical vascular encephalopathy (Binswanger type) in the elderly. J Am Geriatr Soc 1982;30:521-529.
9.- Akiguchi I, Tomimoto H, Suenaga T, Wakita H, Bugka H. Allterations in Glia and Axons in the Brains of Binswanger’s Disease Patients. Stroke 1997;28:1423-1429.
10.- Bennett DA, Wilson RS, Gilley DW, Fox JH. Clinical diagnosis of Binswanger’s disease. J Neurol Neurosurg Psych 1990(3):961-965.
11.- Del Brutto, Rajshekhar V, White Jr AC, Tsang VCW, et al. Proposed diagnostic criteria for neurocysticercosis. Neurology 2001;57:177-183.
12.- Salinas R, Counsell C, Prasad K, Gelband H, Garnet P. Treating neurocysticercosis medically: a review of randomized, controlled trials. Trop Med Int Health 1999; 4(11):13-18.
13.- Salinas R, Prassad K. Drugs for treating neurocysticercosis (tapeworm infection of the brain). Cochrane Database of Systematic Reviews. Issue 2, 2002.
14.- Chotmonkol V. Treatment of neurocysticercosis with a two week course of albendazole. Southeast Asian J Trop Med Pub Health. 1993:24(2):396-398.
15.- Sotelo J, Flisser A. Neurocysticercosis. Practical Treatment guidelines. Cns Drugs 1997;7(1):17-25.
16.- Garcia HH, Gilman RH, Horton J, Martinez M, Herrera G, Altamirano J, Cuba JM, Rios-Saavedra N, Verastegui M, Boero J, Gonzalez AE. Albendazole therapy for neurocysticercosis: a prospective double-blind trial comparing 7 versus 14 days of treatment. Neurology 1997;48(5):1421-1427.
17.- Sotelo J, Jung H. Pharmacolkinetic optimization of the treatment of neurocysticercosis. Review 1998:34(6):503-515.
18.- Del Brutto OH, Campos X, Sanchez J, Mosquera A. Single-day praziquantel versus 1-week albendazole for neurocysticercosis. Neurology 1999;52(5):1079-1081.
19.- Singhi P, Ray Singhi S, Khandelwal N. Clinical spectrum of 500 children with neurocysticercosis and response to albendazole therapy. J Child Neurol. 2000:15(4) : 207-213.
20.- Del Bruto OH. Cysticercosis and cerebrovascular disease: a review. J Neurol Neurosug Psy 1992;55:252-254.
21.- Young Bang Oh, Hoe HJ, Choi SA, Kim DI. Large cerebral infarction during praziquantel therapy in neurocysticercosis.Stroke 1997;28:211-213.
22.- Woo E, Yu YL, Huang CY. Cerebral infaction precipitated by praziquantel in neurocysticercosis: a cautionary note. Trop Geogr Med.1988;40:143-146.
23.- Fong GCY,Cheung RTF. Caution with praziquantel in neurocysticercosis. Stroke 1997;28:1648-1649.
24.- Roman C.G. Impact of Magnetic Resonance Imaging on Vascular Dementia Research. Stroke 1996;27:1269-1273.
25.- Iwamoto T, Kubo H, Takasaki M. Platelet Activation in the Cerebral Circulation in Different Subtypes of Ischemic Stroke and Binswanger’s Disease. Stroke 1995;26:52-56.
26.- Joubert J, Joubert MJ, Lombaard CM. Neurocysticercosis, a comprehensive approach to medical treatment. S Afri Med J. 1985;63:11-14.
27.- Shassha W, van Dellen J, Cakata E. Cysticercosis: an analysisi of 141 cases in South Africa. S. Afri J Epidem. Infect. 1986;1:94-97.
28.- Joubert J, and van As Ad. Rapid resolution of giant cysticercal cysts after administration of praziquantel: a report of 4 cases. S. Afri Med J. 1990;77:154-157.
29.- Thomson AJ. Neurocysticercosis, experience at the teaching hospital of the University of Cape Town. S Afric Med J. 1993;83:332-334.
30.- Bhigjee AI, Sanyika C. Disseminated cysticercosis. J Neurol Neurosurg Psychiatry 1999;66:545-546.
31.- Woo E, Yu YL, Huang CY. Cerebral infarction precipitated by praziquantel in neurocysticercosis: a cautionary note. Trop Geogr Med. 1988;40:143-146.
32.- Bang OY, Heo JH, Choi SA, Kim DI. Large cerebral infarction during praziquantel therapy in neurocysticercosis. Stroke. 1997;28:211-213.
33.- Del Brutto OH, Sotelo J, Roman GC. Therapy for neurocysticercosis: a reappraisal. Clin Infect Dis. 1993;17:730-735.
34.- Salinas R, Counsell C, Prasad K, Gelband H, Gamer P. Treating neurocysticercosis medically: a systematic review of randomized, controlled trials. Trop Med Int Health.1999;4(11):713-718.
La demencia vascular es un tipo frecuente de demencia. Su prevalencia está en torno al 13%-19% siendo el tipo de demencia más frecuente en personas mayores de 85 años. La demencia vascular puede dividirse en dos subtipos principales: la demencia multiinfarto (una afectación cortical) y la enfermedad de Binswanger (una afectación subcortical).
La enfermedad de Binswanger se caracteriza por la lesión microvascular de las arteriolas penetrantes medulares que se internan en la sustancia blanca y de las lenticuloestriadas que irrigan los ganglios basales. La clínica comienza con un enlentecimiento global de las funciones mentales, apatía, desorientación y, en su fase final, síntomas y signos del síndrome pseudobulbar (incontinencia de esfínteres, piramidalismo, labilidad emocional y disartria). Una causa de este tipo de demencia es la neurocisticercosis.
La neurocisticercosis es la enfermedad parasitaria más frecuente del sistema nervioso central, siendo una patología neurológica relativamente común en América Latina, Africa y Asia La prevalencia exacta de la neurocisticercosis es muy dificil de determinar por la inespecificidad de sus manifestaciones clínicas y por la falta de una prueba que pueda ser utilizada en estudios epidemiológicos a gran escala.
Se han descrito una gran variedad de signos neurológicos focales en enfermos con neurocisticercosis, cerebral siendo los más frecuentes el déficit motor, la liberación piramidal, la ataxia cerebelosa, los signos de disfunción de tallo cerebral y los movimientos involuntarios. Estas manifestaciones suelen seguir un curso progresivo, pero en algunos casos los signos focales aparecen de forma súbita, especialmente cuando ocurren infartos cerebrales secundarios a angeitis cisticercosa.
Algunos enfermos tienen signos de hipertensión endocraneal, a veces con crisis convulsivas, y signos focales o alteraciones mentales.
En la mayoría de los casos la hipertensión endocraneal sigue un curso lentamente, a veces con episodios súbitos de pérdida de conciencia relacionados con movimientos de la cabeza (síndrome de Bruns), cuando la causa de la hidrocefalia es un cisticerco en el IV ventrículo. Otras formas de neurocisticercosis que se asocian con hipertensión endocraneal son los quistes subaracnoideos gigantes y la encefalitis cisticercosa. Esta última es una forma particularmente grave de neurocisticercosis que ocurre como resultado de la invasión masiva del parénquima cerebral por de cisticercos que ocasionan una intensa reacción inflamatoria; la encefalitis cisticercosa es más frecuente en niños y mujeres jóvenes y se caracteriza por deterioro de la conciencia, crisis convulsivas, disminución de la agudeza visual, cefaleas, vómitos y papiledema. La neurocistiscercosis se diagnostica mediante pruebas de neuroimagen e inmunológicas. La presencia de cisticercosis extracerebral facilita el Fuera del SNC los cisticercos pueden localizarse en el globo ocular donde pueden detectarse mediante un examen oftalmoscópico, en los músculos esqueléticos o el tejido celular subcutáneo, donde pueden identificarse mediante radiografías simples o incluso mediante la palpación.
La TC y la IRM en pacientes con neurocisticercosis meníngea suelen revelar hidrocefalia, captación anormal del contraste en las leptomeninges basales, quistes subaracnoideos e infartos cerebrales. En los pacientes con infarto, la angiografía puede mostrar una estenosis segmentaria de arterias intracraneales de mediano calibre. Con excepción de las lesiones quísticas, la mayoría de los hallazgos de neuroimagen en la neurocisticercosis meníngea no son específicos y pueden observarse en otro tipo de infecciones del sistema nervioso
Tanto el praziquantel como el albendazol son potentes drogas cestocidas praziquantel puede acabar con el 60% al 70% de los cisticercos parenquimatosos tras 15 días de tratamiento. Además el control de las crisis convulsivas es mucho mejor si los enfermos son tratados con drogas cestocidas. También se ha documentado una marcada mejoría en los signos neurológicos focales de los pacientes con quistes gigantes. Sin embargo, hay formas de neurocisticercosis que no deben tratarse con cestocidas, como. la encefalitis cisticercosa ya que estas drogas pueden agravar el edema cerebral. Los enfermos con hidrocefalia y quistes parenquimatosos o subaracnoideos se tratan con cestocidas una vez que la hidrocefalia ha sido resuelta mediante la implantación de un sistema de derivación ventricular. En los pacientes con quistes gigantes o ventriculares, el tratamiento cestocida debe valorarse los potenciales riesgos de su empleo.
La administración simultánea de corticosteroides durante el tratamiento cestocida está sujeta a debate. Se emplean para disminuir los efectos adversos debidos a la destrucción de los parásitos. Sin embargo existe unanimidad en cuanto a la conveniencia de emplearlos en caso quistes subaracnoideos gigantes, quistes ventriculares y quistes localizados en la médula espinal. En estos casos,deben ser administrados antes, durante y después del tratamiento cestocida para disminuir el riesgo de infartos cerebrales, hidrocefalia o edema medular.
En este artículo, el Profesor Foyaca nos presenta el estudio de siete pacientes con manifestaciones clínicas de demencia vascular y pruebas de neuroimagen compatibles con neurocisticercosis y enfermedad de Binswanger y una revisión de su tratamiento, llegando a la conclusión de que esta enfermedad Binswanger es más común de lo pensado y de que no hay suficientes pruebas de que el tratamiento con praziquatel sea beneficioso, por lo que debe ser desaconsejado.
Ni que decir tiene que la demencia o demencias, ese síntoma clínico que está presente en un buen número de enfermedades que comprometen al SNC, representa/tan una de las formas de expresión patológica más preocupantes y que amenazan lo más característico y diferencial de nuestra especie: las facultades mentales del intelecto y de la cognición. Es por esto que cualquier intento por entender mejor, e incluso curar o paliar mencionado padecimiento merece nuestra atención.
De las numerosas series clínico-patológicas publicadas en la literatura en relación con las enfermedades que cursan con demencia (Sourander y Sjögren, 1970; Marsden y Harrison, 1972; Jellinger 1976; del Ser T, 1987; Tong Q, 1990; Harrell L 1993; Kondo N, 1995; Bermejo Pareja 2002 entre muchas otras) parece que está perfectamente asumido que las enfermedades que presentan una mayor prevalencia en los países occidentales son las "Demencias preseniles y seniles" (Alzhemier), seguidas casi a la par de las "Demencias vasculares". A éstas dos grupos principales se les sumarían las Enfermedades Degenerativas y los Procesos expansivos (tumores primarios y metastásicos). Pero la lista, todos lo sabes, se debería completar con un sin fin de procesos metabólicos, y aquellos otros que ocasionan hidrocefalias, traumatismos, infecciones del SNC etc.
Lo que de forma original Foyaca-Sibat e Ibañez-Valdés nos exponen en éste trabajo es una serie, no desdeñable, de 7 casos donde existe una coincidencia de Demencia Vascular tipo Binswanger con Neurocisticercosis activa.
En nuestro medio la prevalencia de la Cisticercosis como causa de Demencia resulta muy limitada (Bermejo Pareja y col en una serie de 338 casos clínicos de demencia únicamente la diagnosticaron en 3 ocasiones) pese a que nuestro país, sin considerarse dentro de los endémicos, sigue incluyéndose
entre los de baja frecuencia (Pitella 1997). Garcia-Albea (1989) revisó hace años la información epidemiológica de 52 pacientes estudiados en el Hospital "12 de Octubre" de Madrid con Cisticercosis y concluyó que las áreas de mayor riesgo en España son las comunidades rurales más occidentales de la península aunque parecía que la incidencia estaba remitiendo si se comparaba con la previa a los años 70, en gran parte debido a las mejores condiciones sanitarias y de desarrollo social que habían experimentados éstas áreas en los últimos años. Aunque no debemos olvidar que, es en éstas mismas Comunidades donde se siguen declarándose también los únicos casos de Triquinosis de nuestro país http://193.146.50.130/ve/EDO2002.htm
Recientemente Font Puig (1999) describe 4 casos de Neurocisticercosis en España de pacientes inmigrantes procedentes de países donde si está presenta ésta infección de forma endémica. Y finalmente solo mencionar como comparación que en Italia Carangelo y col (2001) ha publicado también un caso de Neurocisticercosis calificándolo como de extremada rareza.
En ninguno de los casos descritos hasta la fecha en nuestro medio se ha hecho mención a la coincidencia expuesta por Foyaca-Sibat e Ibañez-Valdés de Enfermedad de Binswanger con Neurocistercosis, aunque después de lo leído y considerando su mayor experiencia creemos que debería intentarse abundar en las hipótesis que nos formulan.
En el resto de países occidentales, donde la prevalencia de éste tipo de infección es casi desconocida, el interés por las enfermedades infecciosas que pueden ocasionar una clínica de demencia sí ha vuelto a atraer la atención de cuantos tienen que tratar con este tipo patologías y mayoritariamente de la opinión pública general, dada sobre todo la alarma ocasionada por el incremento de las Encefalopatías Espongiformes. Al describir S. Prusier el agente etiológico de ésta enfermedad como la proteína del prión o PrP transmitida a la especia humana desde una epizootia padecida por animales bovinos y ovinos, parece que el resto de demencias de causa infecciosa (neurosífilis, cisticercosis etc.) quedarían circunscritas a poblaciones con escaso desarrollo en el control de su salud pública; o como también apunta recientemente Carpio (2002), debido al incremento de los movimientos poblacionales de emigración. Para éste autor, como para muchos otros, la aproximación más eficaz a la solución de las teniasis y de la cisticercosis sería la prevención, que debería ser la mayor preocupación de los servicios de salud pública en aquellos países menos desarrollados. Aunque paradójicamente, en los países considerados como más desarrollados se están produciendo ocasionales alarmas de salud que nos dejarían bien a las claras que nunca es bueno rebajar la guardia.
Como resume Jellinger (1976), las bases anatómicas de las demencias vasculares son: la encefalopatía arteriosclerótica con infartos lacunar (grandes) o multiinfarto; la atrofia cortical granular resultante de los desordenes microcirculatorios locales; la enfermedad cardiovascular hipertensiva con afectación mixta tanto cortical como subcortical, y la forma más rara afectación solo subcortical o atrofia arterosclerótica de la sustancia blanca hemisférica conocida también como Enfermedad de Binswanger.
La encefalopatía arteriosclerótica subcortical o Enfermedad de Binswanger, cuyo diagnóstico hasta hace poco resultaba exclusivo de las autopsias, con el desarrollo de los estudios de imagen (TAC, RMN, PET) ha comenzado a incrementarse dado que cada vez es más frecuente reconocer éste tipo de encefalopatía crónica en pacientes hipertensos de mediana edad (Hojer-Pedersen, 1987). No pensamos por tanto que resultara difícil en lo sucesivo indagar la relevancia de mencionada coincidencia: Binswanger-Cisticercosis y tener presente que, como apunta Popper (1982) pese a la rareza de éstos casos en Europa, deben incluirse de forma obligada en todo diagnóstico diferencial de las demencias.
Como comentario final a ésta revisión no quiero dejar pasar por alto la interesante imagen que los autores nos muestran de lo que describen como "Activación de microglía". Nos han privado de conocer qué técnica histoquímica o inmunohistoquímica han realizado para poder caracterizar de forma tan precisa lo que efectivamente parecen "el tercer elemento de Cajal". Incluso, siendo más exigentes, hasta el poder ver con mejor detalle esa imagen. Queremos pensar que llegar a ver esa activación de la microglía ha sido posible con una técnica de carbonato de plata débil de Del
Río Hortega y animamos a aquellos patólogos que tengan que afrontar un estudio necrósico en el que concurran las coincidencia descritas por Foyaca-Sibat e Ibañez-Valdés observen, como ellos, el estado proliferativo o no de mencionados macrófagos como posible indicio de respuesta a la infección.
http://www.ispub.com/ostia/index.php?xmlFilePath=Journals/ijn/vol1n2/ncc.xml
http://www.scienceinafrica.co.za/2002/june/worm.htm
Comentario de Ramón Diaz-Alersi. Hospital Puerto Real. Cadiz. España
Comentario de E. Moro Rodríguez. Universidad Rey Juan Carlos. Facultad de Ciencias de la Salud. Madrid. España.
