Indice del volumen
Volume index
Comité Editorial
Editorial Board
Comité Científico
Scientific Committee
PSEUDOSEIZURES AND EPILEPSY IN NEUROCYSTICERCOSIS.
*Foyaca-Sibat H., **Ibañez-Valdés L de F.
*Department of Neurology, **Department of Family Medicine. Faculty of Health Sciences.
University of Transkei. Umtata. South Africa.
foyaca @ intekom.co.za
Rev Electron Biomed / Electron J Biomed 2003;1(2):79-87.
Comment Reviewer Dr. Marco T. Medina. Profesor de Neurologia Director Postgrado de Neurologia Universidad Nacional Autonoma de Honduras
Comment Reviewer Dr. Roberto Cuan Ravinal. Departamento de Patologia. Faculdade de Medicina de Ribeirão Preto. USP-Ribeirão Preto. Brazil
ABSTRACT.
We studied 32 rural patients from the poorest regions in South Africa, diagnosed as epilepsy due to neurocysticercosis presenting pseudoseizures. We found that the common clinical characteristics of this series and its psychological profile such as: duration of events, history of sexual abuse in females, absent of focal neurological signs, vocalization in the middle of the seizures, and lack of post-ictal symptoms were very useful for its differential diagnosis, and the possible difference between the clinical features and psychological profile of those patients and others without PS. Finally, some advices for the management of this condition by family doctors are suggested.
KEY WORDS:
Psychogenic seizure, epileptic seizure, calcified neurocysticercosis.
INTRODUCTION.
Neurological problems are estimated to comprise 10 to 15 percent of a family physicians workload, and headaches, seizures, and behavior disorders frequently are encountered in primary care, neurology, and psychiatry settings. The specialty of family practice is vitally interested in all aspects of neurological disease. History taking in neurology and performance of the neurological examination are essential skills. Emphasis on good diagnostic and therapeutic skills and appropriate consideration of biopsychosocial factors must be considered as priorities, therefore we need to learn to distinguish in our thinking and in our living, and surely in our practice those expressions of organic lesions of the central nervous system (CNS) from those due to its functional disturbances that characterize neurological, psychiatric, or neuropsychiatry patients in order to provide them a better treatment. To differentiated epileptic seizures (ES) from pseudoseizures (PS) or vice versa that knowledge is crucial, however if both manifestations coincide on the same patient probably other diagnostic tool should be required.
PS are sudden changes in behavior that resemble epileptic attack but lack organic cause, and are also known by conversion seizures, disociative seizures, hysterical seizures, psychogenic seizures, and nonepileptic seizures (Bowman E, and Markand O.1999; Bowman ES and Coons PM. 2002). PS are often misdiagnosed and represent the opposite end of the spectrum from seizures that mimic psychiatric disorders without organic cause and an expected EEG changes. Accurately distinguishing PS from EP and other illnesses is difficult because of the breadth and overlap of symptoms seen in each condition and because of the frequent co-occurrence of PS and epilepsy (Bowman ES, 1968). Subjects with PS exhibited trauma-related profiles that differed significantly from those of epileptic comparison subjects and closely resembled those of individuals with a history of traumatic experiences (Fleisher W et al, 2002). PS patients frequently report a history of physical and sexual abuse, and traumatic experience is considered part of the mechanism for producing dissociation and may be a manifestation of dissociative disorders, especially when a history of sexual or physical abuse is documented. (Harden CL ,1997) A controversy currently exists regarding the significance of dissociation and conversion in the pathogenesis of PS. After the abolition of the term "hysterical neurosis" from the current diagnostic systems, these seizures were diagnosed as either Dissociative Disorders (ICD-10) or in the DSM IV as Somatoform disorder, most often of conversion type. The significantly higher incidence of dissociation in the patients with PS suggests dissociation in the pathogenesis of these seizures (Prueter C, 2002).
Neurocisticercosis (NCC) is a parasitic infection of central nervous system (CNS) caused by the larval stage (Cysticercus cellulosae) of the pig tapeworm Taenia solium. This is the most common helminthes to produce CNS infection in human being. The occurrence of acquired epilepsy or the syndrome of raised intracranial pressure in a person living in or visiting a region where taeniasis is endemic or even in one living in close contact with people who have taeniasis should suggest a diagnosis of cysticercosis; the NCC may remain asymptomatic for months to years and sometimes its diagnosis is made incidentally when neuroimaging is performed. Symptoms and signs are related both to the parasite which can show a different biological behavior from one place to another, and to the inflammatory-inmunological response of the host. NCC is the most common cause of acquired epilepsy worldwide and most of the patients taking phenytoin or carbamazepine for a proper control of their seizures, respond very well (Foyaca and Ibanez, 2002; Foyaca and Ibanez, 2003). For interested peoples, other aspects concerning to NCC from our region are available on line (Foyaca et al, 2001; Foyaca and Ibanez, 2002; Foyaca and Ibanez, 2003).
Significant advances have been made in the diagnosis and treatment of epilepsy over the past decade. With the advent of electroencephalographic video monitoring, physicians are now able to reliably differentiate epilepsy from other conditions that can mimic it, such as PS. Many new antiepileptic drugs have become available in recent years. The ketogenic diet has resurfaced as a treatment option in certain types of epilepsy and the vagus nerve stimulator, approved in 1997, represents a completely new treatment modality for patients with seizures not controlled by medications, and finally epilepsy surgery is now a well-documented and effective treatment for some patients with intractable epilepsy.
Former Transkei (FT) was one of the three administrative authorities of the so-called independent homelands (Ciskei, Transkei and the Cape Provincial Administration under different apartheid governments) it is currently named: region D and E of Eastern Cape Province and it is also the poorest region of South Africa, that region serves as a labor reservoir for other wealthier provinces, with men leaving behind women and children whilst they seek and find employment elsewhere. FT (Figure 1) has the most relevant indices of poverty and underdevelopment and show a remarkable limited access to employment, cash income, primary education, safe and clean water, proper toilet facilities, proper refuse disposal, electricity, and telecommunication. Some communities still do not have easy access to any health facility. (Mahlalela X, et al, 1997-2002).

Figure 1: Current view of the former Transkei (Photo by X. Mahlalela)
Poverty is defined by the United Nations as the denial of opportunities and choices most basic to human development to lead a long, healthy, creative life and to enjoy a decent standard of living, freedom, dignity, self-esteem and respect from others. Poverty in our region is far from being eradicated and because NCC is a fruit of poverty, we believe that eradication of NCC is also far to be reached.
The aim of this study is to identify a psychological profile of a group of patients with epilepsy NCC-related presenting PS and to detect the possible difference between the clinical features and psychological profile of patients affected by PS and ES NCC-related and those patients in whom EP are associated with NCC only and have been before- reported (Foyaca and Ibanez, 2001, 2002, 2003)
PATIENTS AND METHOD.
At the beginning, all patients were assisted by one of us (I-VLdeF) at Mhlakulo Health Center, which is one of the biggest rural clinics at the FT. From September 1998 to February 2003 all selected patients were referred to neurology out patient clinic at Umtata General Hospital (UGH) and admitted for this study. UGH offers neurology tertiary care services to 6,4 million peoples for surrounding rural areas. We agreed with those patients that no action will be taken against them to modify their economical or disability grant status after concluded this study, whatsoever happened.
We included female and male patients, 14 years of age and older who had all developed EP fulfilling the International League Against Epilepsy criteria for epilepsy, and the radiological criteria for calcified NCC (considering multiples intraparenchymal calcifications between 2 to 10 mm in patients from endemic regions as patonogmonic, until proven otherwise), who experienced at least one attack of PS per month.
Patients were excluded for the following reasons: seizures caused by clear precipitants such as: alcohol, hyperglycemia, or hypoglycemia; we also excluded patients with previous medical history of head injury, stroke, brain tumor, cortical dysplasia, hyponatremia, hypomagnesemia, hypoparathyroidism, cardiac arrhythmias, heart failure, and history of medication taken on the past six months such as: theophylline, meperidine hydrochloride, isoniazid, antipsychotic drugs, alkylating agent, beta-lactam antibiotics, tricyclic antidepressants, acyclovir, beta-blockers and decongestants; also pregnant or breastfeeding women, and patients with any medical condition that might interfere with the interpretation of the results of this study. At screening, all patients had a physical examination, including a detailed neurological examination done by one of us (FSH), routine laboratory test including hematology, urinalysis, urea and electrolytes, glucose, plain skull X-rays, CT Scan of the head, and a 32 channel digital EEG.
Seven patients presented PS that we could not distinguish clinically from EP therefore their anticonvulsant medication were rapidly tapered to provoke seizure, if the seizure did not develop, other serial maneuvers including 24 hours sleep deprivation followed by hyperventilation and suggestion with intravenous saline injection (2 patients) were done. Diagnosis of PS was considered when their "typical" seizures did not change the background EEG activity under observation plus others clinical features of PS.
All patients granted written informed consent before entering the study.
RESULTS.
Study population.
In total, 32 patients were eligible for this study among several hundreds of people with epilepsy due NCC. The demographic and clinical characteristic of patients in each group are summarized in Table 1.
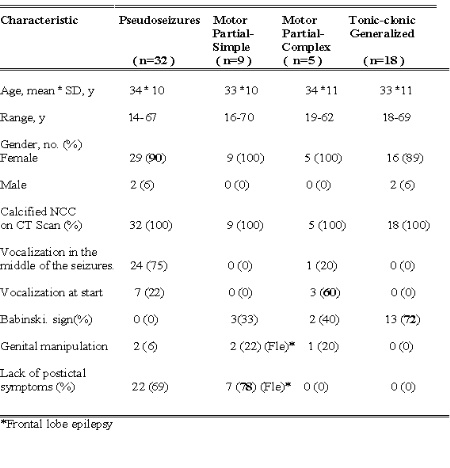
Table 1 Baseline demographic and clinical characteristic of pseudoseizures and epileptic attacks.
All patients presented radiographic signs of calcified NCC on CT Scan (Figure 2), and, signs of other stage of the parasite were also observed but the predominant finding was no less than five calcified lesions fulfilling the radiographic criteria for calcified NCC at the brain cortex or in the sub-cortical regions.
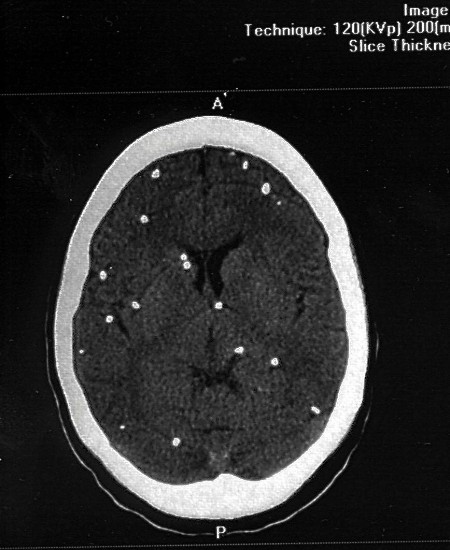
Figure 2: Multiple calcified lesions due to NCC on CT S can of the brain.
In this series, 37 % of patients (all women) were on disability grant program for epilepsy, and that cash income was the only way for alleviation their requirements and poverty, however evidence of malingering on this group could not be proved.
Eighty five percent of the studied female patients were single mothers or married women living alone with their children while their husband were working in gold mines very far away from home, and only contact between them happened on December every year.
Seventeen female patients from our series complained of a previous history of sexual abuse, and 14 of them physical abuse also. Members of their own family raped 10 women, and 11 mentioned other members of their families that have had been raped during their early youth. According to information obtained from this group families suffered deeply when one of their member was raped, and 6 peoples were also murdered. Usually their father or the mother became chronically depressed, alcoholic, and their socio-economical situation became remarkably deteriorated; for 5 patients to talk about this topic was rejected, and each refused to accept psychiatry or psychological referral because of financial or transport problems (25%), because they did not consider it necessary (18%), or for other reasons.
Maximal duration of tonic-clonic ES was 95 seconds and for PS was 904 seconds, and minimal duration was 45 seconds for EP, and 18 seconds for PS. See Table 2.
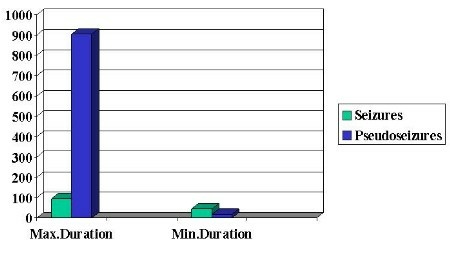
Table 2: Duration of the events in seconds.
Psychic manifestations were present in different group: frontal lobe epilepsy (FLE), Tonic-clonic generalized (TCG) or Grand Mal epilepsy, Partial Complex Motor Seizure (PCS), and PS as can be seen on Table 3:
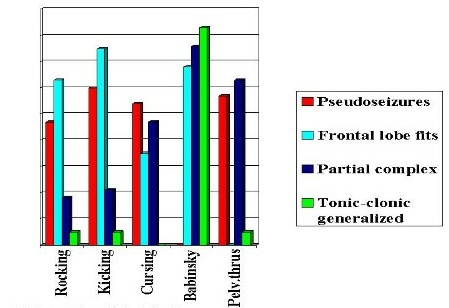
Table 3: Other clinical findings.
-
Rocking: PS=47, FLE=63; PCS=18, TCG=5;
Kicking: PS=60, FLE=75, PCS=21, TCG=0;
Cursing PS=54, FLE=35, PCS=47, TCG=0;
Babinski: PS=0, FLE=65, PCS=76, TCG=83;
Pelvic thrusting: PS=57, FLE=0, PCS=63, and TCG=5,
other dissociative symptoms of depersonalisation and desrelization were present only in patients with PCS/PS.
In general patients complained of PS revealed higher percentage of Somatoform Disorders and Cluster B Personality Disorders. The occurrence of PS mimicking generalized tonic-clonic ES was documented only on illiterate peoples.

Table 4: Psychic manifestations in both groups.
Three patients complained of auditory hallucinations, two had focal complex motor seizures also and the third one TCG and paranoid schizophrenia, all presented calcified NCC on the basal ganglia without active or calcified lesion of NCC on the temporal lobe. EEG under provocative saline solution done in two patients did not show changes on the background activity during the test (Figure 3)
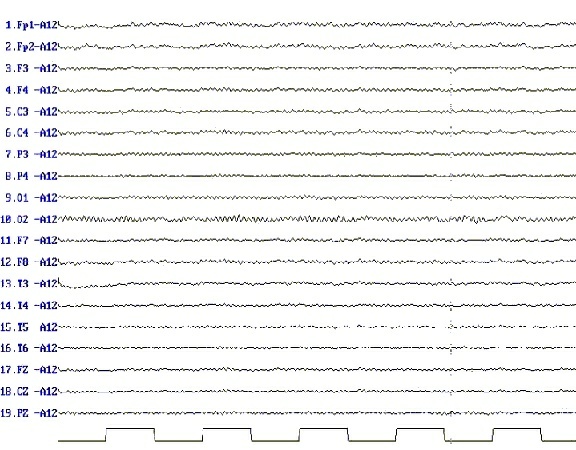
Figure 3: No changes of the background activity on the EEG during provocative saline infusion and the occurrence of pseudoseizures.
COMMENTS.
At the FT, ES are the commonest clinical expression of calcified NCC as we have had been before published (Foyaca and Ibanez, 2001, 2002, 2003)but the associated PS is related with other functional disturbances no usually present in patients with epilepsy and NCC alone.
Symptoms of complex partial seizures, especially the reactive automatisms and subjective abnormal sensations, are difficult to differentiated from dissociative symptoms of depersonalization, derealization, and alteration of consciousness can be misinterpreted as symptoms of seizure disorder, for the other hand some nonspecific EEG abnormalities and possibly structural NCC findings can contribute to reinforce this diagnostic impression therefore when they are present, in absent of other reliable diagnostic tools, both "organic" and "functional" disturbances should be treated at the same time. We agree that bilateral motor seizures with retained consciousness are rare and often mistaken for PS (Ashkenazi A, 2000).
When a realistic threat of physical or sexual assault to a member of their family involved in the problem is revealed, is important the role for family therapy skills in the evaluation and treatment of PS (Griffith JL. et al, 1998)
Some patients did not improved from the occurrence of PS probably because of lack of more specialized medical treatment, and others discontinued their treatment (including antiepileptic drugs) in spite of our personal agreement, probable because of fear to loss their disability grant among other limitations, and also because of ignorance, superstition, and poor health education. Many patients found solace in becoming and remaining neurological ill, thus defense mechanism of denial, dissociation, introjections, identification, and symbolization contributed to the patient’s symptom picture and to their adaptation to traumatic life events. Bringing the unconscious psychogenetic elements into conscious awareness is an important aspect of the treatment of dissociative disorders (Nemiah, J.C, 1991) and may be assayed by family physician if there is not other choice.
Using anti-epileptic drug in patients with PS before its confirmation was a common problem in other series (Gunatilake SB, 1997; Benbadis SR, 1999) but not for us because all patients from this series presented ES and were treated accordingly.
Auditory hallucinations, perception without external stimulus, are paradigmatic symptoms of the schizophrenic patients, and can be present in disorders such as: Alzheimer’s Disease, epilepsy, deafness, tumors of the temporal lobe, and toxic psychosis, usually due to disturbances of the left temporal lobe, limbic, and paralimbic areas. We could not demonstrated the source of the hallucinations in our series but based on our observations we have hypothesized that hallucinations could be secondary to hyperactivity of the basal ganglia (thalamus and striatum) since that mechanism was before-published (Benbadis SR et al, 1995).
Most of our patients were on disability grant program for epilepsy before joining us for this study and we believe that their "atypical seizures" were not simulated for earning money and we did not assume that those events were purposeful acts to get attention. In malingering, the patient has intentional and obvious goals, such as financial compensation or avoidance of duty or school, evasion of criminal prosecution, or obtaining of drugs. Such goals may resemble secondary gain in conversion symptoms, but with the distinguishing feature being the conscious intent in the production of the symptoms, mechanism that we could not proved.
Why more ladies than gentlemen on this series? Because there are more females than males living in Transkei (for migratory reasons) and also because women are more susceptible than men to develop this kind of somatoform disorder therefore increased incidence and prevalence of PS. Charcot and Freud emphasized the sexual aspects of the seizure as has the current interest in childhood sexual abuse. Major mood disorders and severe environmental stress, especially sexual abuse, were common problems among our patients should be considered in every case. From case studies and review of the literature the author believes that psychogenic seizures in women express rage, fear, and helplessness against the dominant and abusive male rather than sexual conflicts. Emphasizing the aggressive component of seizures does not minimize the traumatic effects of sexual abuse but rather includes it as leading to rage and helplessness (Rosembaum, 1999)
We performed EEG under provocative saline solution for extremely limited number of patients because we consider that deceptive diagnostic tests are justified only in exceptional situations. The use of provocative saline solution in that way is fundamentally deceptive, requiring the physician to intentionally and directly lie to the patient, causing the patient to believe that the administered solution caused his seizures, provocative saline infusion compromises the fiduciary obligation of truthfulness, is inimical to patient autonomy, is undignified, and risks grave harm to patient trust in physicians, however if nondeceptive alternatives are not available and the difficulty of distinguishing malingerers can not be solved then we have not choice and deceptive diagnostic testing should be implemented. Without such deception, the test might be useless (Burack and Back, 1997)
Management.
From our personal experience, sometimes those patients have to be treated by family doctors. Under those circumstances we strongly recommended to be very patient, very kind, and also very gentle, we advice do not accuse anybody of malingering or deliberately faking the seizures under any circumstances, and always advised to get counseling. We suggest do not forget they inability for controlling their PS and for proper socialization and its impact on their families, friends and other members of the community. We learned that it is a good practice to understand their disabilities, frustrations, and to identify their hopes. It is very important to define the underlying causes and the triggering factors for PS such as: rage, fear, and panic among others, and to contribute in the healing process of emotional hurts and their emotional control; to provide an ideal psychological support and to address an adequate management of stress, emotional upset, or physical illness are also recommended; do not named those patient as hypochondriac and to explain clearly why they are unaware of the source contributing to the events, when it will be appropriated. When patients are having PS to keep them safe, just as would be done when they are having ES is strong recommended, if the diagnosis of PS is clear-cut then leaving the patient alone until it is over, keeping the environment calmed and free of starling noises is the best choice. When the PS is over, try to elicit some kind of respond from the patient. Never use suggestions by hypnotic procedures if you have not enough expertise for it. Physical abuse on patients having PS must be damned forever. It is very successful to encourage patients for exploring they own feelings and assisted in learning to cope with the feelings in new ways. Patients with history of attend to suicide are not suitable for this group. If there is not a good response in a due time, the diagnosis must be revised.
CONCLUSION.
The clinical differentiation of PS from epileptic attacks in patients with NCC is particularly difficult and sometimes almost impossible if 24-hour videoEEG monitoring techniques are not available, but duration of events, history of sexual abuse in females, focal neurological signs, vocalization in the middle of the seizures, and lack of postictal symptoms can be very useful for its differential diagnosis, however if the patient presents PS, temporal lobe epilepsy, other types of epileptic seizures because of NCC, and an associated conditions such as factitious disorder and malingering then confirmation PS can not be reached. Under exceptional circumstances those patients can be treated by their family physician if some specialized advices are adjusted.
REFERENCES.
Ashkenazi A, Kaufman Y, Ben-Hur T. Bilateral focal motor status epilepticus with retained consciousness after stroke. Neurology 2000;54:976-978.
Benbadis SR, Stern E, Frith C, Cahill C, Holmes A, Grootoonk S, Seanward J, Mckenna P, Chua SE, et al A functional neuroanatomy of hallucinations in schizophrenia. Nature 1995;378:176-179.
Benbadis SR. Eur Neurol 1999;41(2):114-115.
Bowman ES. Pseudoseizure. Psychiatr Clin North Am 1968;21:649-657.
Bowman E, Markand O. The contribution of life events to pseudoseizure occurrence in adults. Bull Menninger Clin 1999;63:70-88.
Bowman ES, Coons PM. The differential diagnosis of epilepsy, pseudoseizures, dissociative identity disorder, and dissociative disorder not otherwise specified. Bull Menninger Clin 2000;64:164-80
Burack JH, Back AL. Provoking nonepileptic seizures: The ethic of deceptive diagnostic testing. Hasting Center Report 1997;27:24-34.
Fleisher W, Staley D, Krawetz P, Pillay N, Arnett JL, Maher J. Comparative study of trauma-related phenomena in subjects with pseudoseizures and subjects with epilepsy. Am J Psychiatry 2002;159:660-663.
Foyaca SH, Ibañez V.LdeF, Awotedu A, Fernandez MC. Neurocysticercosis in critical stage. Third International Congress of Critical Care Medicine on Internet.
Available from: http://www.uninet.edu/cimc2001/comunicaciones/foyaca/index.html
Foyaca SH, Ibañez VLdeF. Clinical trial of praziquantel and prednisone in rural patients with neurocysticercosis presenting recurrent epileptic attacks. The Internet Journal of Neurology 2002;1(2).
Available from:
http://www.ispub.com/ostia/index.php?xmlFilePath=Journals/ijn/vol1n2/ncc.xml
Foyaca SH, Ibañez V. LdeF, Awotedu A, Fernandez MC. Neurocysticercosis in the former Transkei. 7th Internet World Congress for Biomedical Sciences INABIS 2002.
Available from:
http://www.inabis2002.org/poster_congress/area_01/01011/010117.pdf
Foyaca SH. Tapeworm and the brain. Science in Africa. June 2002;XVIII:(3).
Available from: http://www.scienceinafrica.co.za/2002/june/worm.htm
Foyaca SH, Ibañez VLdeF. Intraventricular neurocysticercosis. II Virtual Congress of Neurosurgery.
Available from: http://www.neuroc.sld.cu/papers/tl-neurocys.htm
Foyaca SH, Ibanez-Valdes LdeF. Intraventricular neurocysticercosis in HIV positive patients. The Internet Journal of Neurology.2003;2(1).
Available from: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijn/vol2n1/ncc.xml
Foyaca S.H, Ibanez V. LdeF. Vascular dementia type Binswanger’s disease in patients with active neurocysticercosis. Electron J Biomed 2002;1(1):1-12
Available from: http://www.uninet.edu/biomed/rebio/reb/2002/n1/foyaca.html
Foyaca S.H, Ibanez V.LdeF. Enfermedad de Binswanger en pacientes con neurocisticercosis activa. IV Internet Congreso de Psiquiatria Interpsiquis 2003.
Available from: http://www.psiquiatria.com/interpsiquis2003/9638
Foyaca SH, Ibanez-Valdes LdeF. Binswanger’s Disease and neurocysticercosis. The Internet Journal of Neurology. 2003;2(1).
Available from: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijn/vol2n1/bins.xml
Griffith JL, Polles A, Griffith ME. Pseudoseizures, families, and unspeakable dilemmas. Psychosomatics 1998; 39:144-153.
Gunatilake SB, De Silva HJ, Ranasinghe G. Twenty-seven venous cutdowns to treat pseudostatus epilepticus. Seizure 1997; 6:71-72.
Harden CL. Pseudoseizures and dissociative disorders: a common mechanism involving traumatic experiences. Seizure 1997;6:151-155.
Mahlalela X, Rohde J, Meidany F, Hitchinson P, Bennett J. Primay Health Care in the Eastern Cape province. 1997-2000 EQUITY PROYECT. South Africa Department of Health.
Nemiah, J.C. Dissociation, conversion and somatization. In A. Tasman & S.M Goldinger (Eds), American Psychiatry Press review of psychiatry. Washington DC: American Psychiatric Press 1991. Vol 10, pp 248-260.
Rosenbaum M. Why Women? Psychosomatics. 2000;41:147-149.
